ABSTRACT
One of the most important strategies of the restorative treatment is the valuation and re-establishment of occlusal vertical dimension (OVD). This phase must not be neglected, because the decrease or increase of OVD causes damage to teeth, muscles, joint and difficult the patient’s swallowing and phonation. This paper presents the treatment of a patient with loss of occlusal vertical dimension with dental wear caused by parafunctional habits. The planning for oral rehabilitation was initially making occlusal overlay bilateral splints in acrylic resin for the recovery of the intermaxillary distance and after the patient’s adaptation and muscular stability to the new occlusal condition, the definitive rehabilitative treatment evolved into direct restorations in composite resin associated with all-ceramic crowns reinforced by lithium disilicate.
INTRODUCTION
During the life of a person all teeth suffer a certain wear due to functional activity.1Occlusal wear has mostly been attributed to attrition, erosion, abrasion, and parafunctional habits.2,3 Besides that, diet and diseases such as gastric reflux, congenital abnormalities, and eating disorders are important contributors to excessive occlusal wear.4 Excessive wear of anterior dental elements is a fact of high influence on the smile’s esthetics and harmony.3-5 As cases become more complex, aspects related to the patient’s occlusion re-establishment must be observed, including the recovery of the occlusal vertical dimension (OVD), which is defined as the vertical distance between two points, one in maxilla and one in mandible, when the occlusal surfaces are in contact.6-8 One of the most important aspects in facial appearance involves the Occlusal Vertical Dimension, as the esthetics of the face is affected by facial form and facial height.9 When a patient presents decreased OVD, because of advanced tooth abrasion, attrition, or tooth loss, its facial appearance is aged due to the decrease of the lower third of the face, lips intrusion, drop of the nose and can also bring phonetic and masticatory disorders and possible involvement of the temporomandibular joint (TMJ) and mastication muscles.5-9 In general, in a situation that there was loss of dental elements or excessive wear of them, the OVD must be recovered before any definitive restorative procedure is executed, it must be done gradually at the beginning of treatment. Temporary acrylic resin crowns, fixed prosthesis or even interim removable prosthesis should be used for initial adaptation, particularly in determining a stable and functional occlusal vertical dimension.5,10 After the creation of an optimum maxillomandibular relationship and the restitution of a restorative space the treatment plan can evolve into a definitive rehabilitation. 11 This paper describes the treatment of a 72-year-old patient who presented decrease in OVD. The treatment consisted in an OVD re-establishment by means of using a provisional device (occlusal overlay bilateral splints) made in acrylic resin. The final restoration occurred after a 60-day follow-up and was made with ceramic crowns in posterior teeth and direct restorations in anterior teeth.
CASE REPORT
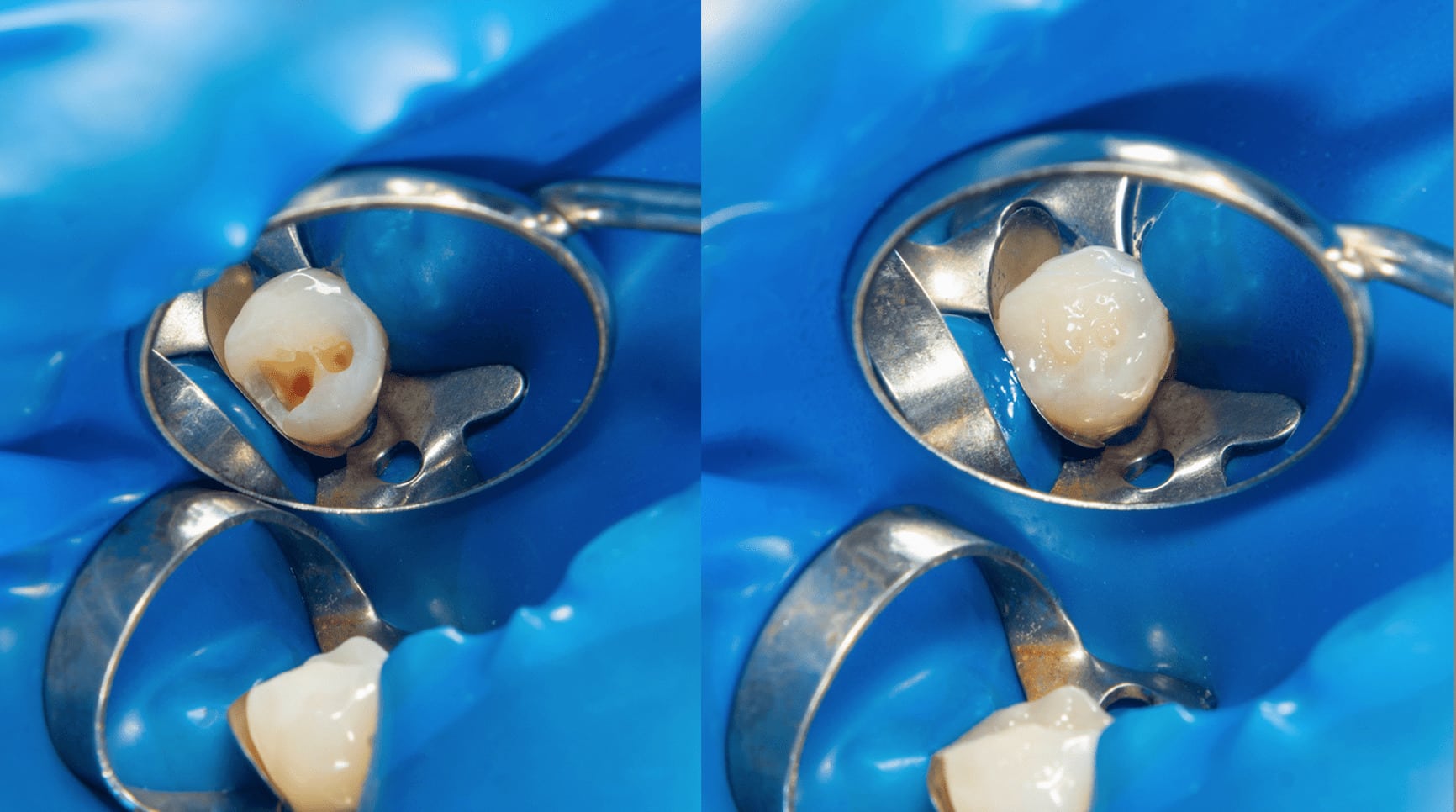
The patient M.I.A., 72 year-old, female, came for a restorative treatment complaining about worn and poor appearance of lower teeth. A thorough history and clinical examination followed, and baseline records were taken on a clinical assessment sheet. During dental evaluation, excessive worn on the mandibular anterior teeth, multiple fractures of restorations, presence of metal-ceramic crowns on the teeth 12, 11, 21, 22, 46, 47, 36, 37, 38 and absence of teeth 35 were noticed. It was also noticed a loss of anterior guidance and reduction of OVD. Patient reported grinding teeth habit, with sporadic episodes of painful symptoms. Periodontal condition was stable, with normal mucosa color and no tooth mobility (Figure 1). Impressions were made with alginate and cast models were manufactured, reproducing the current status of the patient’s occlusion. The OVD was assessed using a Willis Bite Gauge.12 In order to do that, patient was positioned in an erect posture, and asked to look forward performing the occlusion in maximum intercuspal position, gently touching the lips. The lower third of the face (base of the nose to up on the chin) was measured without pressing the soft tissues. After that, this measurement was compared to the measurement of the middle third of the face (distance between inner commissure of the patient’s eye and the labial commissure). It has been found that these two distances was not coincident; meaning that OVD was reduced and the discrepancy was 3 mm. The re-established OVD was also verified on the patient’s physiologic rest position (facial muscle relaxation), satisfactory phonetics, and aesthetics and swallowing ability.13 The intermaxilary distance of the re-established OVD (defined previously) was transferred to the casts models by bite registration with condensation silicon. Two portions of dense material were manipulated and positioned bilaterally on the occlusal surface of lower posterior teeth. The Willis Bite Gauge12 set on the re-established OVD was positioned on the patient’s chin, without pressing the soft tissues. The patient was told to occlude and stay motionless when the upper fixing rod of the Willis Gauge touched the base of the nose, so it could wait for the final solidification of the material. At the end of the procedure we had the models and the height registration that would be re-established, which was about 3mm (Figure 2).
Figure 1 Periodontal condition stable prior to treatment.
_______________________________________________________________________________________________
Figure 2 Final height registration.
_______________________________________________________________________________________________
The casts models and the bite registrations were sent to the prosthetic for confection of bilateral lower splints in acrylic resin. These devices overlaid the entire occlusal surface of molars, premolars and lower canines and the buccal and lingual surfaces just below the prosthetic equator of these teeth, reproducing the anatomical feature of each one (Figure 3). The reason of buccal and lingual surface trespass the prosthetic equator is to position the device in a retentive zone, promoting a more stable fixation of the devices. Bilateral splints could be either attached only by the fit or cemented using temporary material or glass ionomer cement. The advantage of not using a cementation procedure is the ease of cleaning, favoring the oral hygiene and biofilm control. However, by the cementation of the bilateral splints, a more stable condition was obtained and the occurrence of acrylic fractures diminishes. The bilateral splints were fixed upon the occlusal surfaces with glass ionomer chemically activated cement (Figure 4). Following, occlusion was checked and adjustments were performed aiming a harmonic distribution of the occlusal contacts.
Figure 3 Finished and polished restorations, reproducing the anatomical feature of each tooth.
_______________________________________________________________________________________________
Figure 4 Bilateral splints fixed upon the occlusal surfaces with glass ionomer cement.
_______________________________________________________________________________________________
Follow-up appointments were scheduled to accompany the patients’ adaptation to the re-established OVD. The acrylic splints remained in position for 60 days being monitored in aspects related to TMJ discomfort, chewing, swallowing and speech. After this period of time allied to the patient's tolerance to the new OVD, the definitive restorative procedures were initiated.
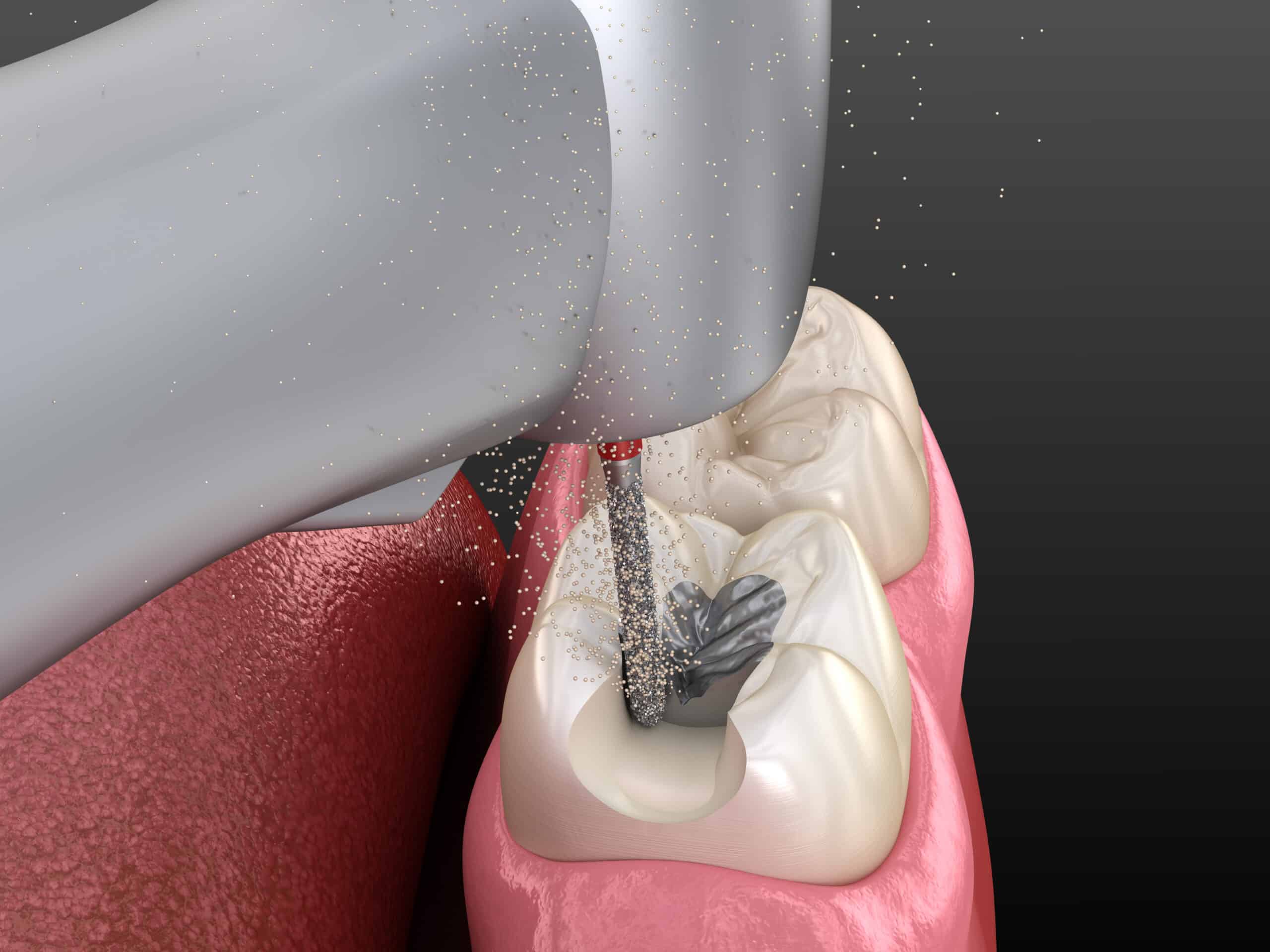
Restorative procedures of the upper posterior teeth were performed with resin composite. The 3 mm increase in OVD was distributed between the two arcades. Resin composite was inserted in a way to increase 1.5 mm teeth height. This procedure caused the distribution of the restored height in both arcade, so it would not be concentrated only in the lower arch, which could negatively affect the teeth appearance resulting in extremely elongated lower teeth (Figure 5 & Figure 6). Occlusal adjustments on the lower splints were required to promote occlusal balance. To facilitate the restorative procedures of lower anterior teeth, the use of a silicone guide was chosen. Impressions were taken with alginate and cast models were manufactured. The dental cast was waxed (teeth 33, 32, 31, 41, 42 and 43) and a silicone guide was made (Figure 7 & Figure 8). The selected color was A3 to dentin and A3.5 to enamel. It was made the absolute isolation of the region, the proof and the adaptation of the silicon barrier, a slight beveling of the buccal surfaces was done with a diamond tip drill 1190F, followed by etching of tooth structure using 37% phosphoric acid for 30 seconds on enamel and 15 seconds on dentin, application of primer and adhesive, curing and the composite resin was inserted, using the stratification technique (Figure 9). After the conclusion of the restorations the isolation was removed and the finish and polishing were performed. A check of the occlusion was made with the patient sitting occluding in M.I.P (Maximum Intercuspal Position) and simulating the protrusive and lateral movements. The next step was the removal of the lower crowns, refinishing the preparation and confection of single provisionals. Then we proceeded with the impression of the tooth preparing and the implant with addition silicon, bite registration with self-curing red acrylic resin and color selection of A3 Vita scale for the confection of ceramic crowns reinforced by lithium disilicate. At the proof the checking of occlusion was performed with the patient sitting occluding in M.I.P. and simulating the protrusive and lateral movements, after adjusting the crowns returned to the prosthetic for glaze applying. Previously to cementation, the inner surface of the crowns was etched with 37% phosphoric acid for 60 seconds to remove any remaining grease, after being washed and dried they were etched with 10% hydrofluoric acid for 20 seconds and after a further washing and drying received the silane application. It was performed the relative isolation of the field and insertion of the retraction cord for containment of the gingival fluid, the tooth surface was etched with 37% phosphoric acid for 15 seconds, washed and dried and the application of dual adhesive system was made, at first the application of the activator, after the primer followed by the catalyst (3M ESPE). The resin cement dual RelyX ARC (3M ESPE) was manipulated and the crowns were placed, the cement excesses and retraction cords were removed and the set was cured for 60 seconds on each surface. Final aspects after increasing OVD and restorative procedures are shown in Figures 10-12 .
Figure 5 Occlusal adjustments on the lower splints to promote occlusal balance.
_______________________________________________________________________________________________
Figure 6 Final occlusal adjustments on the lower splints.
_______________________________________________________________________________________________
Figure 7 Aspect of the silicone guide.
_______________________________________________________________________________________________
Figure 8 Concluded waxing.
_______________________________________________________________________________________________
Figure 9 Stratification technique.
_______________________________________________________________________________________________
Figure 10 Intraoral anterior view of teeth after treatment.
_______________________________________________________________________________________________
Figure 11 Intraoral superior occlusal view of teeth after treatment.
_______________________________________________________________________________________________
Figure 12 Intraoral inferior occlusal view of teeth after treatment.
_______________________________________________________________________________________________
DISCUSSION
The rehabilitation of patients with extensive occlusal wear is complex and difficult to solve, becoming thus one of the biggest challenges of dentistry.5,14,15 Rehabilitation procedures are increasingly sought after by patients. As these cases become more complex, aspects related to patient’s OVD re-establishing must be observed because its recovery is of great importance for making prosthetic works,8 although it’s not taken into consideration in most of the cases. Physiologically all teeth suffer wear due to functional activity, however, this process can be accelerated and intensified when there is loss of posterior elements causing overloading of the remaining anterior teeth and increasing the potential to wear,7 occlusal disorders and parafunctional habits such as bruxism.16-18 According to glossary of prosthodontic terms, bruxism is the parafunctional grinding of teeth, or an oral habit consisting of involuntary rhythmic or spasmodic nonfunctional gnashing, grinding, or clenching of teeth, in other than chewing movements of the mandible, which may lead to occlusal trauma. There is no single cause that is responsible for bruxism, but some etiologic factors include: morphological factors such as dental occlusion, psychosocial factors such as stress and certain personality characteristics, patho-physiological factors (i.e., diseases, trauma, genetics, smoking, alcohol, caffeine intake, illicit drugs and medications) and sleep disorders (sleep apnea and snoring).19
Dental enamel is the first structure that receives the parafunctional load of bruxism. When the mandible shifts from side to side, heavy horizontal forces are applied on the teeth, which are not well-accepted and which increase the chances of damage to the teeth and/or supportive structures. Besides, bruxism occurs in eccentric positions, which causes the application of heavy forces to a few teeth, not many, as occur normally in functional activity, when the mandible is at or near the centric occlusion position.19 The loss of tooth tissue due to this parafunction is associated with tooth sensitivity, excessive reduction of the clinical crown’s height and possible changes in OVD, because of the intensity of tooth wear.10,20-22] Wear is considered pathological when it is excessive for the patient's age, requiring treatment because of functional and/or aesthetics reasons.13,23 The loss of tooth structure does not necessarily imply the loss of occlusal vertical dimension,10,24 so for determining if there was change of OVD, aspects such as loss of posterior containment, wear rate should be observed, as well as phonetic evaluation through the use of sibilant sounds, the interocclusal distance and facial appearance.7,10,13 The increasing of OVD causes dental contact during emission of sibilant sounds, difficulty of lip closure, difficulty swallowing and pain,25 whereas the decreased OVD, when the teeth are in occlusion, cause an exaggerated closure that is detrimental to the temporomandibular joint, excessive lip contact and angular cheilitis.7,26
The first step in case of excessive wear in the anterior region consists in re-establishing the occlusal vertical dimension, which should be performed to recover the height of the lower third of the face and create interocclusal space to allow the occlusal reconstruction, anterior and canine guidance.7 The occlusal vertical dimension was defined in 1989 by the Academy of Denture Prosthetics as the height of the patient’s facial profile measured by two points selected in the maxilla and mandible when the teeth are in occlusion and the rest vertical dimension as the height of the patient’s facial profile measured by two points when the mandible is in the rest position.6 When the mandible is in rest position, there is a vertical space between the occlusal surface of the maxillary and mandibular teeth, which is called freeway space (FWS) that is on average 2-3 mm.27 Several techniques have been used to measure OVD. However, no method is scientifically accurate being the most used the method of facial, phonetic and metrical proportions.12,28 Some aspects make the OVD re-establishing a complex procedure, one of them is the fact that no technique for OVD determining has been scientifically proven superior than anyone to be used during the restoration of OVD 29 and the other is the fact that the postural rest position is not fixed,7 suffering variation with pain stimuli, temperature, habitual posture of the head, the body, occlusal interferences, disorders, emotional state, among others.
The WILLIS method advocates equal distances between the base of the nose to the chin (lower third of the face) and labial corner to the inner commissure of the eye (middle third of the face), when the teeth are in maximum intercuspal. An instrument was developed in the format of letter "L" - Willis compass, which appeared on the market in 1930, to facilitate these measurements.12,30 This method is convenient, accurate and practical because it requires no sophisticated or costly equipment to be applied, besides being easily mastered by the operator.12 However, it is consensus among the authors that the use of more than one proposed method for OVD determination is an option to ease the weaknesses of each method.31 A proper planning of a prosthetic rehabilitation should not attribute the re-establishing of occlusal vertical dimension (OVD) to new prostheses at the risk of the patient doesn’t adapt to a new condition of vertical dimension. The restoration of OVD should be obtained gradually and, for this, we can use provisional removable partial dentures, also called therapeutic and often involving the need for coronary coverage, with prostheses of type "overlay".5,11 They are reversible, easy to adjust, restore VD and stabilize the occlusion, providing a preliminary analysis of the neuromuscular system’s response and the phonetic and aesthetic evaluation before definitive changes in the dentition. The rehabilitative treatment requires that the restoration of OVD go through a trial period, with the use of these interim prostheses. Some authors mention the re-establishing splint of vertical dimension.8 In patients with excessive dental wear it acts as a device that determines the correct OVD, providing to mandible a positioning where the occlusal contacts are comfortable, this device can be considered a provisional prosthesis of type overlay.32 There is no consensus about the period of the patient’s adaptation to the new VD, but according to the literature review the minimum is an interval of 04 weeks, where aspects such as discomfort of TMJ, chewing, swallowing, speech and aesthetics will be evaluated.1,13 The loss of OVD must be treated in a patient who has the habit of teeth grinding, even if the patient doesn’t present painful symptomatology, because this parafunction is capable of destroying the aesthetics and function of the masticatory apparatus.23
CONCLUSION
Tooth wear causes dimensional changes in facial morphology and OVD decrease. The correct determination of occlusal vertical dimension represents a factor of success in the rehabilitation treatment, because if it is not properly restored, keeping it decreased, there may be production of damage to the teeth, muscles, TMJ, swallowing and speech. The treatment using occlusal overlay bilateral lower splints in acrylic resin provided the re-establishing of acceptable standards of function, aesthetics, and comfort, and can be considered an adequate rehabilitative technique in situations of OVD reduction. The patient that was asymptomatic remained so, the rehabilitation treatment did not cause any painful symptoms to the patient, the presence of eventual episodes of painful symptomatology prior to treatment may be associated with loss of OVD, once there was a remission of these symptoms after its restoration. The obtained result was quite satisfactory because after the end of treatment the patient was highly satisfied with the recovery of the aesthetic previously committed.
ACKNOWLEDGEMENT
Elaine Gomes Rodrigues de Assis,1 Fl vio Henrique Baggio Aguiar,1 Renata Pereira,1 Marilia Mattar de Amoedo Campos Velo,2 Debora Alves Nunes Leite Lima,1 Maria Cecilia Caldas Giorgi3
1Department of Restorative Dentistry, University of Campinas,
2Department of Operative Dentistry, Endodontics and Dental Materials, University of S?o Paulo, Brazil
3Department of Health Sciences, State University of Amazonas, Brazil
Correspondence: Maria Cecilia Caldas Giorgi, Department of Health Sciences, State University of Amazonas, Av. Carvalho Leal, 1777, Cachoeirinha, Manaus, AM, CEP: 69065-001, Brazil, Tel 55-923878-4361
Received: December 01, 2017 | Published: February 14, 2018
Citation: Assis EGR, Aguiar FHB, Pereira R, Velo MMAC, Lima DANL et al. (2018) Re-Establishment of an Occlusal Vertical Dimension: A Case Report. J Dent Health Oral Disord Ther 9(1): 00336. DOI: 10.15406/jdhodt.2018.09.00336
REFERENCES
- Song MY, Park JM, Park EJ. Full mouth rehabilitation of the patient with severely worn dentition: a case report. J Adv Prosthodont. 2010;2(3):106−110.
- Harpenau LA, Noble WH, Kao RT. Diagnosis and management of dental wear. J Calif Dent Assoc. 2011;39(4):225−231.
- Dietschi D, Argente A. A comprehensive and conservative approach for the restoration of abrasion and erosion. Part I: concepts andclinical rationale for early intervention using adhesive techniques. Eur J Esthet Dent. 2011;6(1):20−33.
- Moshaverinia A, Kar K, Aalam AA, et al. A multidisciplinary approach for the rehabilitation of a patient with an excessively worn dentition: a clinical report. J Prosthet Dent. 2014;111(4):259−263.
- Humel MMC, Takahashi JMFK, Paulillo LAMS, et al. Direct restorative treatment of anterior weared teeth after re−establishment of occlusal vertical dimension: a case report. Gerodontology. 2012;29(4):299−307.
- The glossary of prosthodontic terms. J Prosthet Dent. 2005;94(1):1−105.
- Abduo J, Lyons K. Clinical considerations for increasing occlusal vertical dimension: a review. Aust Dent J. 2012;57(1):1−10.
- Ergun G, Yucel AS. Full−Mouth rehabilitation of a patient with severe deep bite: A clinical report. J Prosthodont. 2014;23(5):406−411.
- Orenstein NP, Bidra AS, Agar JR, et al. Changes in Lower Facial Height and Facial Esthetics with Incremental Increases in Occlusal Vertical Dimension in Dentate Subjects. Int J Prosthodont. 2015;28(4):363−370.
- Bachhav VC, Aras MA. Altering occlusal vertical dimension in functional and esthetic rehabilitation of severely worn dentition. J Oral Health Res. 2010;1:2−8.
- Soares CJ, Pizi EC, Fonseca RB, et al. Direct restoration of worn maxillary anterior teeth with a combination of composite resin materials: a case report. J Esthet Restor Dent. 2005;17(2):85−91.
- Webb R, Bater M, Brennan PA. Use of a Willis bite gauge to measure intercanthal distance. Br J Oral Maxillofac Surg. 2007;45(7):598.
- Geerts GAVM, Stuhlinger ME, Nel DG. A comparison of the accuracy of two methods used by pre−doctoral students to measure vertical dimension. J Prosthet Dent. 2004;91(1):59−66.
- Sato S, Hotta TH, Pedrazzi V. Removable occlusal overlay splint in the management of tooth wear: a clinical report. J Prosthet Dent. 200;83(4):392−395.
- Pruthi G, Jain V, Agnihotri H. Rehabilitation of a Severely Worn Dentition using Fixed and Removable Partial Overdenture Prostheses. Int J Prosthodont. 2011;1:59−64.
- Smith BG, Robb ND. The prevalence of toothwear in 1007 dental patients. J Oral Rehabil. 1996;23(4):232−239.
- Khan F, Young WG, Daley TJ. Dental erosion and bruxism. A tooth wear analysis from south east Queensland. Aust Dent. 43(2): 1998;117−127.
- Gargari M, Ceruso FM, Prete V, PujiaA (2012) Prosthetic−restorative approach for the restoration of tooth wear. Vdo increase, rehabilitation of anatomy andfunction and aesthetic restoration of anterior teeth. Case report. Oral Implantol (Rome) 5(2−3): 70−74.
- Reddy SV, Kumar MP, Sravanthi D, Mohsin AH, Anuhya V (2014) Bruxism: a literature review. J Int Oral Health 6(6): 105−109.
- Fishman LS. Dental and skeletal relationships to attritional occlusion. Angle Orthod. 1976;46:51−63.
- Varrela J. Dimensional variation of craniofacial structures in relation to changing masticatory−functional demands. Eur J Orthod. 1992;14(1):31−36.
- Alfadda SA. A conservative and reversible approach for restoring worn teeth: a clinical report. J Prosthet Dent. 2014;112(1):18−21.
- Chacona RL. Enamel loss and occlusal vertical dimension. Causes and considerations for treatment. Dent Today. 2003;22(4):92−97.
- Gopi Chander N, Venkat R. An appraisal on increasing the occlusal vertical dimension in full occlusal rehabilitation and its outcome. J Indian Prosthodont Soc. 2011;11(2):77−81.
- MacAvoy SK, Jack HC, Kieser J. Effect of occlusal vertical dimension on swallowing patterns and perioral electromyographic activity. J Oral Rehabil. 2006;43(7):481−487.
- Turrell AJW. Clinical assessment of vertical dimension. J Prosthet Dent. 1972;96(2):79−83.
- Pleasure MA. Correct vertical dimension and freeway space. J Amer Dent Assoc. 1951;43(2):160−163.
- Yamashita S, Shimizu M, Katada H. A Newly Proposed Method to Predict Optimum Occlusal Vertical Dimension. J Prosthodont. 2015;24(4):287−290.
- Rivera−Morales WC, Mohl ND. Relationship of occlusal vertical dimension to the health of the masticatory system. J Prosthet Dent.1991;65:547−553.
- Willis FM. Esthetics of full denture construction. J Am Dent Assoc. 1930;17(4):636−642.
- Millet C, Leterme A, Jeannin C. Vertical dimension in the treatment of the edentulous patient. Rev Stomatol Chir Maxillofac. 2007;111(5−6):315−330.
- Mehta SB, Banerji S, Millar BJ, et al. Current concepts on the management of tooth wear: part 3. Active restorative care 2: the management of generalised tooth wear. Br Dent J. 2012;212(3):121−127.