HOW DO WE ASSESS FULLY THE VITALITY OF THE PULP?
Diagnosis is defined as ‘the process whereby the data obtained from questioning, examining and identifying a disease, condition or injury from its signs and symptoms. These diagnosis are documented and are evaluated by the dentist to identify deviations from the normal.
Pulp Vitality test is one of the facets of Endodontics. A pulp test should provide a simple, objective, standardized, reproducible, non-painful, non-injurious, accurate, and inexpensive way of assessing the condition of the pulp. It helps as a guide for Endodontists to identify the diseases of the pulp and the apical periodontitis. If the pulp is deemed to be compromised as a result of the diagnostic testing, then Endodontic treatment, or indeed extraction may be needed.
This post provides clinician a review of clinical pulp vitality test.
TYPES OF PULP VITALITY TEST
A. ELECTRIC PULP TESTING
The procedure electric pulp testing is performed with an electric pulp tester (EPT). This monopolar device flows high-frequency electrical current from the probe tip through the tooth creating an electric stimulation. While the current is flowing through the tooth, viable A-delta nociceptive fibers will be stimulated, resulting in a tingling or “zinging” sensation to the patient. This test requires that the tooth to be well-dried and isolated. It is recommended to dry the tooth with gauze and place a cotton roll in the vestibule to isolate. Be careful in drying the tooth with an air syringe as this may cause sensitivity in cases of pulpitis. Depending on the EPT used to complete the electrical circuit, a lip clip is placed on the patient, or the patient will holds the metal handle. If a full coverage restoration is present, a fine tip of an explorer or file can be used to contact tooth structure cervical to the crown margin, and the EPT probe tip contacts the instrument. The probe tip is coated with a contact medium, such as petroleum jelly, topical anesthetic or toothpaste. According to some studies, the optimal placement of the tip of the EPT should be on the incisal third for anterior teeth while occlusal third for posterior teeth.
A positive response (meaning the patient felt a sensation) indicates vital pulp tissue, more specifically, viable A-delta fibers. It should be noted this does not indicate pulpal health. A negative response or lack of response indicates necrosis of the pulp (assuming the proper contact was made). The number of the reading is usually of little significance and the test result should be recorded as present or absent. However, a positive response at a high reading that is close to the maximum range of the unit is usually a false positive result.
Errors in the EPT that yield false positive or negative results can occur.
➢ The most common error for a false positive is inadequate tooth isolation. Dry tooth structure that is free from saliva is imperative for an accurate and reliable reading.
➢ Contact with metal restorations and gingival tissue should also be avoided.
➢ A false negative result can occur if the canals are in teeth with immature apices, the teeth have been recently traumatized or extremely calcified.
B. COLD TESTING
Cold testing is one of the two thermal tests. Commonly performed using a refrigerant spray, ice or carbon dioxide snow. This test stimulates A-delta fibers by movement of dentinal tubule fluid according to hydrodynamic theory. The cold temperature causes contraction of the dentinal tubules and an outward movement of the dentinal tubule fluid, resulting in negative pressure. This movement physically affects the odontoblastic processes of odontoblasts that stimulate the A-delta fibers.
Performing the cold test also involves isolating the tooth. While isolation is not as critical as with the electric test, saliva should be wiped away, as this can increase the temperature of the refrigerant spray and may lead to a false negative response. A small cotton pellet on the cotton plier should be enough to saturate the tooth . Compared to a cotton pellet, a cotton swab has less surface area; therefore, it does not adequately transfer cold and should not be used. Also, ensure that the cotton pellet is small enough that it does not contact more than one tooth. The patient should be instructed to notify the clinician if a sensation is felt (for example, by raising a hand) A control tooth should be tested first so the patient knows what a normal sensation feels like. The intensity and duration of the response should be documented.
The response of the suspect tooth is compared to the control tooth to determine the intensity (normal, moderate or severe) and duration (lingering or not). Also keep in mind that thermal tests can be completed on teeth with full-coverage restorations. While metal restorations are conductive and porcelain restorations are insulative, thermal tests can be attempted on both. A positive response indicates vitality. A negative response does not necessarily indicate pulpal necrosis and could be a false negative.
While the cold test is considered an accurate test, false results can still occur. The most common being a false negative on a tooth that has a calcified or receded pulp chamber. This can occur in heavily restored teeth or as patients age. In cases like this, a false result may occur and the patient would most likely not feel a sensation. Radiographs can be used to evaluate the size and position of the pulp chamber to see if a negative response would be expected.
C. HEAT TESTING
The other thermal test is the heat test. Like the cold test, the heat test indirectly stimulates viable A-delta fibers, by movement of dentinal tubule fluid via hydrodynamic theory. Unlike the cold test, the heat test causes expansion of the dentinal tubules, or an inward movement, of the dentinal tubule fluid, resulting in positive pressure and a similar mechanotransduction phenomenon. Compared to the cold test, the nerve response, the patient response, is much lower.
There are a few ways to perform the heat test.
➢ An easy method is to use a dry polishing disk on the tooth, with the friction creating heat on the tooth.
➢ Another way is to isolate an individual tooth with a rubber dam and with a syringe bathe the tooth with warm water.
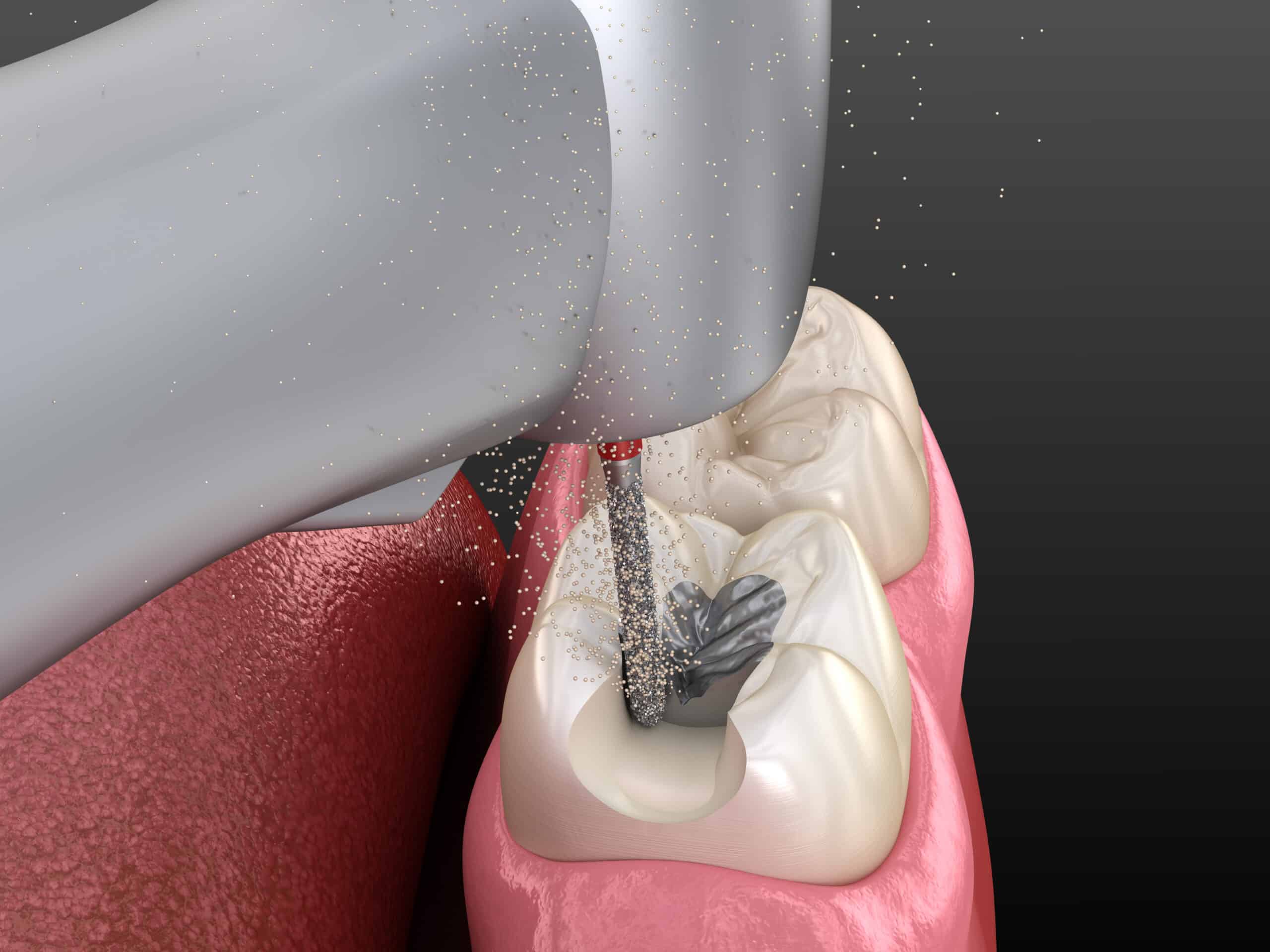
➢The most common way is to heat gutta-percha and apply it to the tooth. White gutta-percha stopping sticks can be heated and applied to the tooth. A light coat of petroleum jelly should be applied to the tooth to avoid gutta-percha adhering to dentition.
➢Heat tests can also be done with heating devices used in the warm vertical compaction method of obturation. Special tips and settings are used to perform the heat test in this manner. The intensity of the reaction and duration should be recorded.
The reasons for false negative and false positive results with the heat test are similar to the cold test, with a calcified or receded pulp chamber being the most common reason for a false negative.
VARYING SENSITIVITIES
All three of these pulpal sensibility tests have varying sensitivities, specificities and accuracies. Studies show cold testing is most accurate (ranging from 84% to 86%) followed closely by the electric test (81% to 82%), with the heat test being the least accurate (70%). Clinicians should be cognizant that even though cold testing is considered most accurate, if the pulp chambers of the teeth being tested appear calcified radiographically, a negative result in itself does not necessarily indicate pulpal necrosis. Two tests should be performed to confirm pulpal necrosis:
A. PERIAPICAL TESTING
The periapical tests include percussion and palpation. Although, these tests do not provide information about the pulp, such as vitality or necrosis, they indicate whether there is inflammation in the periapical tissues.
The percussion test is accurate in identifying and localizing the offending tooth. However, this can only be achieved if the disease has progressed apically to affect the periodontal ligament. The pulp lacks proprioceptors which are needed to localize pain. Therefore, early in the Endodontic disease process, patients have a difficult time localizing the source of pain. The periodontal ligament has proprioceptors, the A-beta fibers, which, when activated via percussion or mastication, transmit a signal to the mesencephalic nucleus in the central nervous system. There, a synapse occurs with a second order neuron that crosses to the contralateral side to reach the thalamus and cerebral cortex for interpretation and localization. The percussion test can be performed by tapping the tooth gently on the incisal or occlusal surface of teeth with the blunt end of an instrument, such as the butt end of a mouth mirror. Light force is needed and the patient should be instructed to inform the dentist of any sensitivity or differences between the tooth in question. A response does not in itself indicate endodontic disease. Occlusal trauma and periodontal disease can result in percussion sensitivity. Percussion should be performed vertically with the long axis, as well as horizontally. If the patient has more sensitivity to horizontal percussion than vertical, and in the absence of other signs or symptoms that would indicate endodontic disease of periodontal origin.
We use palpation to test for periapical inflammation or infection. A gloved index finger and firm digital pressure is applied to the mucosa overlying the root apices from the facial/buccal and lingual aspects. A positive response can be sensitivity, swelling, bony expansion, or a break in the cortical plate. The contralateral side should also be palpated for comparison.
B. Local Anaesthetic Test
When the pain or symptoms are poorly localized or referred, an accurate diagnosis is extremely difficult. Sometimes, patients may not even be able to specify whether the symptoms are from the maxillary or mandibular arch. In cases, and where vitality testing has proved inconclusive, an anesthetic vitality testing can be deemed helpful. Local anaesthetic testing starts with either local infiltration or an intraligamentary injection of the most posterior tooth in the area suspected of the pain. When pain still persists once the tooth has been fully anesthetized, the tooth immediately anesthethized mesial to it, moving distal mesial and so on, until the pain is localized or have disappeared. If the source of the pain cannot be even localized to the upper or lower jaw, an inferior alveolar nerve block injection is given; if pain disappears it indicates involvement of a mandibular tooth. This approach has an advantage over a test cavity, which may cause iatrogenic damage in the long run.
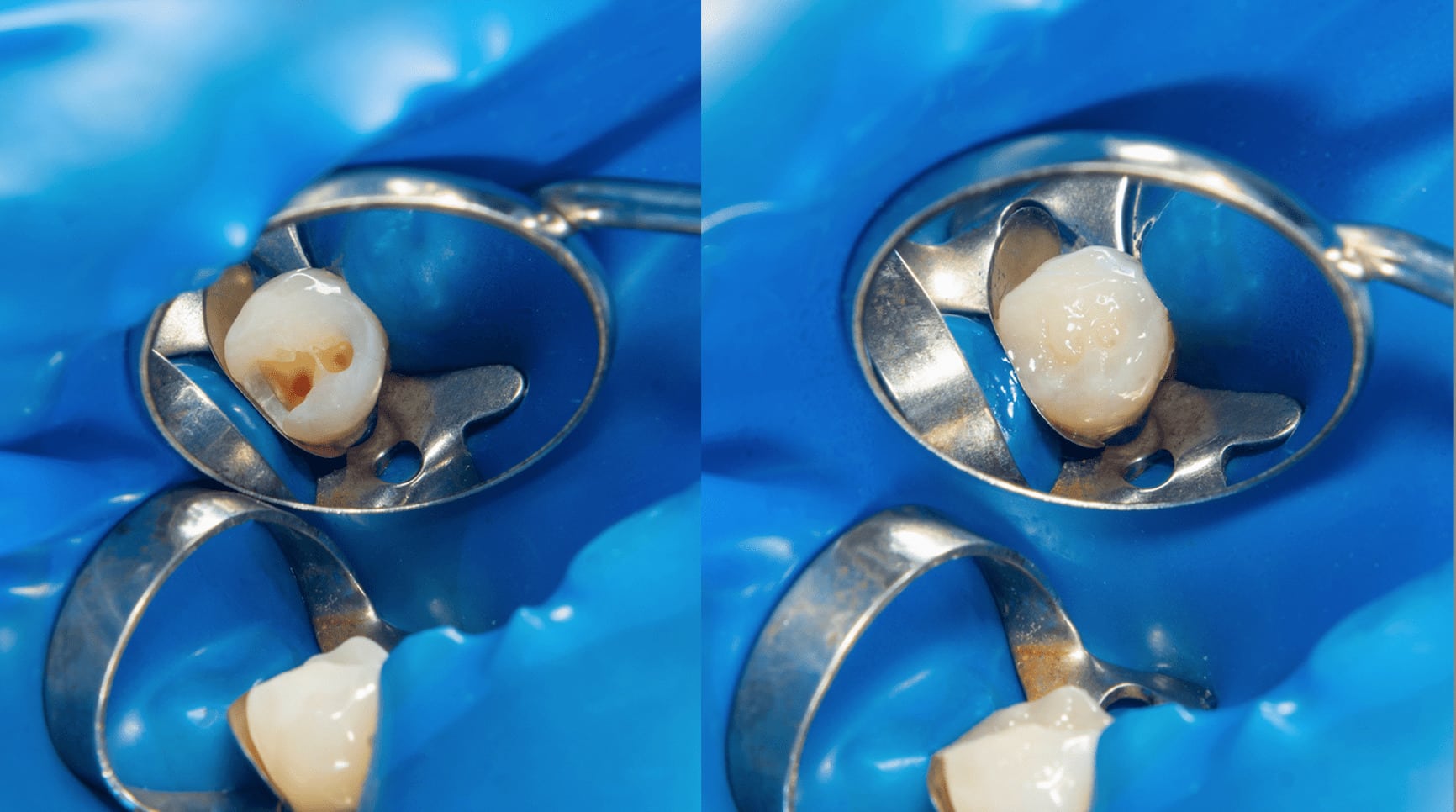
C. Test Cavity Preparation
This test may serve as a last resort in testing for pulp vitality. It is only considered when the results of all other tests have proved inconclusive or to rule out possibility of false positive result. The test cavity is made by drilling with a high speed handpiece and adequate coolant through the enamel–dentin junction of an unanesthetized tooth with good isolation with the use of a rubber dam. The patient is asked to respond if any painful sensation is felt during the drilling procedure. If the patient feels pain once the bur contacts the sound dentin, the procedure is stopped and the cavity is restored.
CONCLUSION:
An accurate assessment of pulp’s vitality is very important in any clinical procedures, more so, when we have to decide whether to recommend root canal treatment or extraction as treatment plan to our patient. The different methods of testing are available for us to wisely use as a diagnostic tool to determine the status of the pulp before we make or decide our treatment plan. Though, pulp vitality testing has its own limitations it has been and still remains a very helpful aid in diagnosis for a probable Endodontic treatment rather than heading to extraction. At any rate, the technology in the practice of Dentistry is continually evolving, and, as such, there will come a time that these methods will have better tools for us to achieve an even higher accuracy in assessing the pulp vitality of our clinical case to provide no error in our judgement with our treatment plan, and, do as much as we can to save our patient's natural tooth.
CONTRIBUTORS:
Dr. Bryan Anduiza - Writer
Dr. Mary Jean Villanueva - Editor
 DMD cEnter is loading...
DMD cEnter is loading...