WHAT ARE OUR OPTIONS IN TREATING NON-VITAL TOOTH?
A non vital tooth is a tooth with a necrotic pulp. A necrotic pulp is suspected when a tooth does not react to vital pulp test such as thermal, electric, or mechanical stimulation and a definitive diagnosis is established only after inspection and probing of the pulp chamber and the root canal. As the infection progresses, the necrotic pulp tissue and the root canal space are infected even in teeth which appears intact. Over time, bacteria in the root canal will induce inflammation outside the tooth, resulting in the formation of an apical abscess, granuloma or cyst.
The objective of treating a non-vital tooth is to remove the necrotic tissue and tissue breakdown by products from the root canal, eliminate the source of infection, seal root canal and establish a functioning tooth in a healthy periodontium. This post serves a review about the different treatment for non vital tooth.
I. GENERAL OVERVIEW OF STEPS IN NON-VITAL TOOTH TREATMENT
The following are the steps in treating a tooth with necrotic pulp with or without a periapical inflammation or when a tooth has been previously root filled and requires re-treatment.
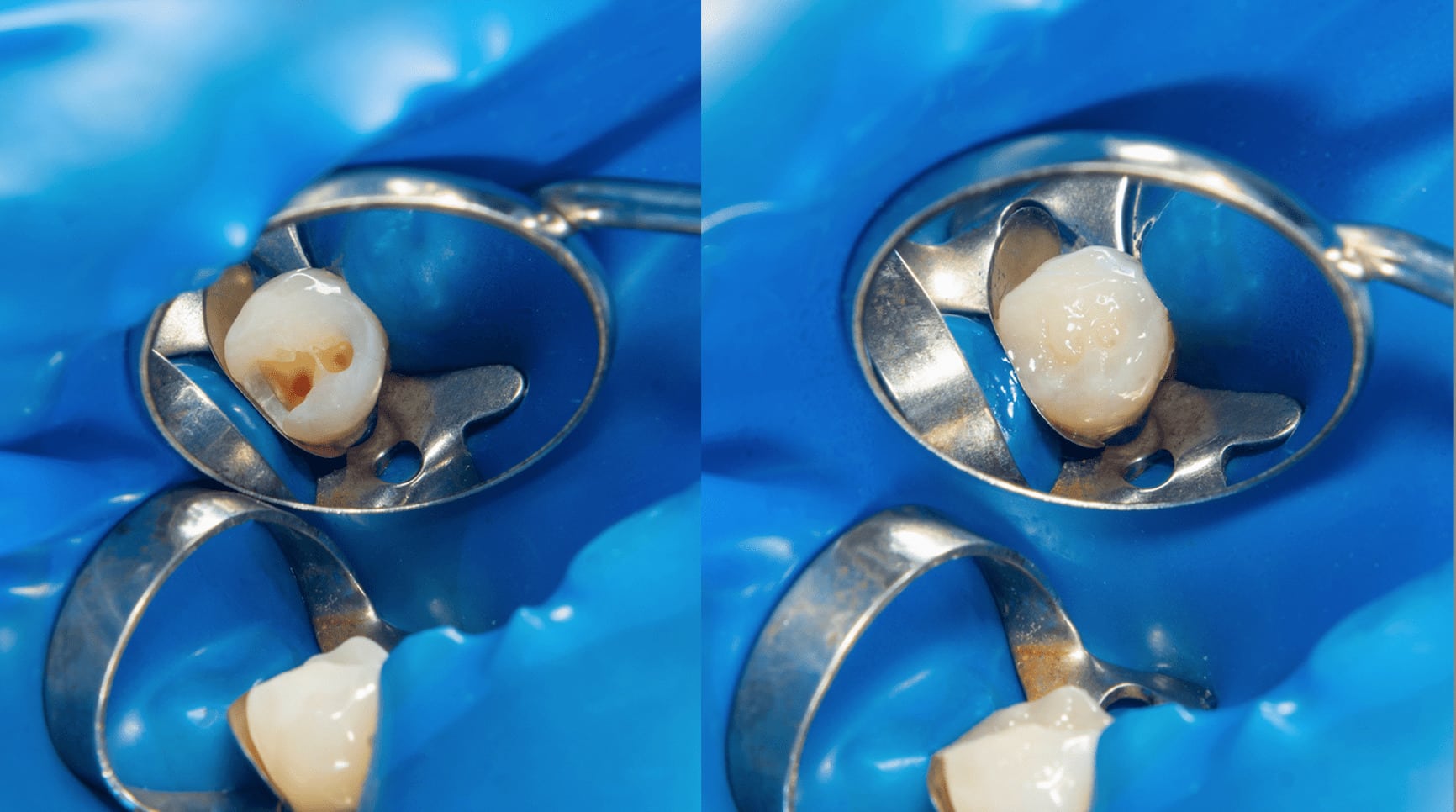
1. Removal of caries, old fillings, etc. and a temporary build-up is done if necessary.
2. Access preparation.
3. Disinfection of the operative field and rubber dam with an antiseptic.
4. The access cavity is filled with a biocompatible antiseptic irrigant such as e.g. Sodium Hypochlorite. A thin endodontic file is carefully moved to a level that is estimated to be 1-2 mm short of the radiographic apex.
5. By means of a radiograph (working length x-ray), taken with the instrument in the canal, the working length is decided. (Usually 1 mm short of the radiographic apex).
6. Cleaning of the canal is started with thin instruments to avoid pushing necrotic, infected material through the apical foramen.
7. Cleaning and shaping of the root canal using copious amounts of irrigation solution.
8. When the cleaning and shaping is finished, the canal is dried and filled with a calcium hydroxide paste.
9. The canal can be filled during the next visit if there are no symptoms, absence of exudate and if fistula occurred, it already healed.
NOTE: If there are symptoms and/or exudate, and/or the presence of a fistula, continue the treatment. This is a sign of remaining infection. When a fistula is still present after 2-3 visits, try to find out if there is another reason for the remaining fistula such as probable root fracture, necrotic neighboring tooth, etc.
II. APEXIFICATION
When the root is not fully developed, an apexification procedure is carried out. After thorough cleaning of the root canal, the calcium hydroxide is left for longer periods of time to give the root development a chance to continue. The intracanal medicament is usually changed after one month. After that, it is left for at least 6 months when a radiographic check-up is done. Usually the canal is cleaned again at this time and the canal is refilled with calcium hydroxide. Next radiographic check is done after another 6 months. If periapical healing and a closure of the root canal have taken place, the permanent root filling can be carried out. If root closure has not taken place, the tooth is checked again after another 6 months. Usually, an apexification procedure will give the desired result. However, in a few cases the root development will not continue and the canal has to be root filled without an apical stop.
NOTE 1: Apexification is a long term treatment that requires good temporary fillings.
NOTE 2: It is the elimination of infection from the root canal and not the action of calcium hydroxide that will make it possible for the body to continue root development. ( It is possible to carry out an apexification procedure successfully without the use of calcium hydroxide. However, a temporary calcium hydroxide root filling is a good means to keep the canal clean and free from infection.)
III. ROOT FILLING
The important thing is to remove bacteria and their products, and tissue debris which can serve as food for bacteria. After that we can obtain healing. However, it is not clinically practical to leave empty root canals. Coronal fillings will leak and infect the empty, cleaned root canal; we need posts for retention, etc. Thus, it is a prerequisite to seal the root canal with a root filling in order to protect the periapical tissues
The root canal can be filled:
➢ When the tooth is asymptomatic.
➢ When there are no clinical signs of infection or inflammation (no exudate, no fistula, no swelling, no redness etc.).
➢ When the canal is properly cleaned and shaped.
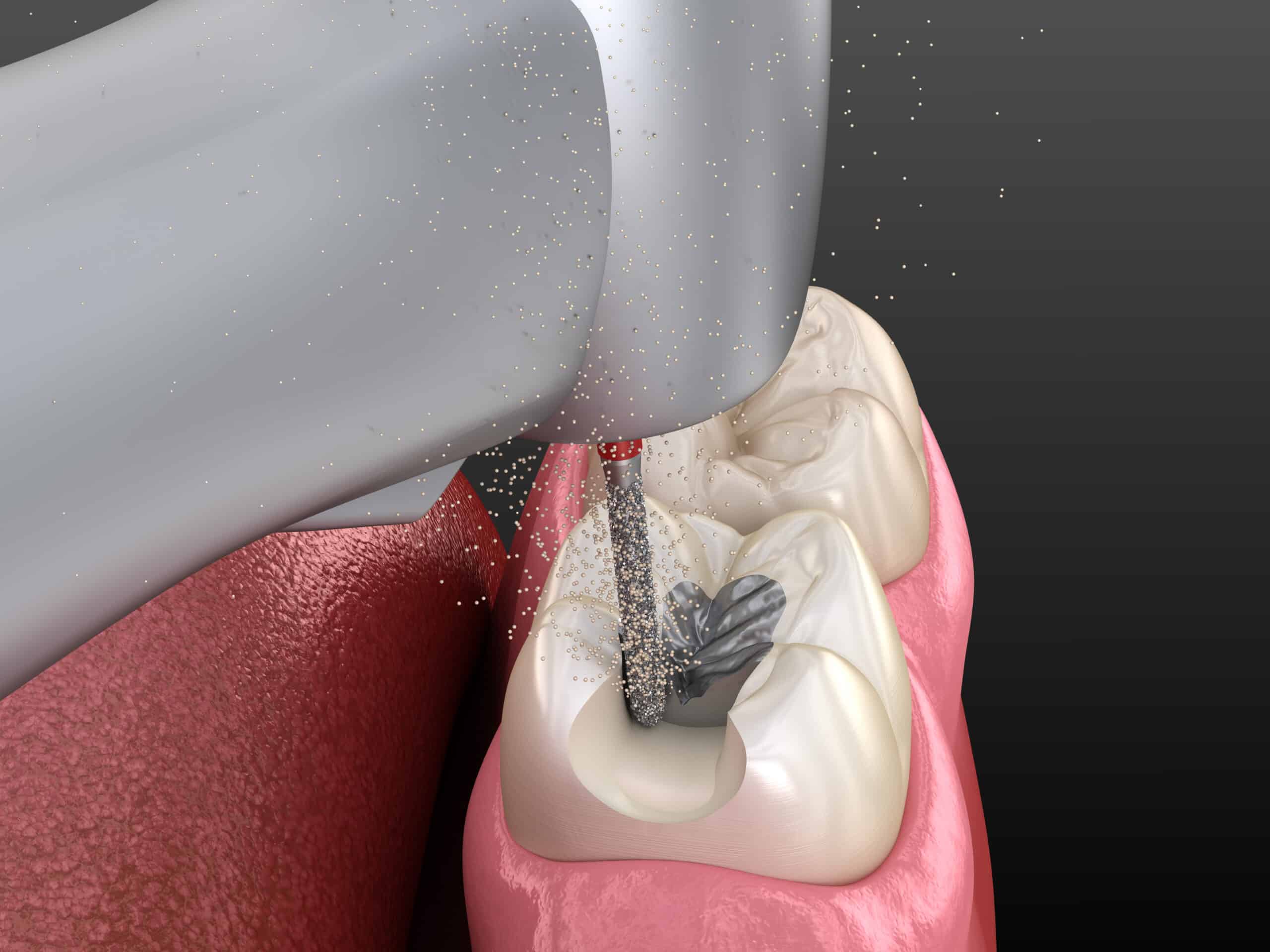
A common method in this is a lateral condensation technique. Lateral condensation is done by pressing a D-11 spreader in the canal along side the cone. Apply pressure apically to push the spreader in as far as possible, and spread from side to side. This side-to-side or, lateral, spreading motion is the basis for the technique’s name. There are many root filling techniques available. However, techniques are mainly based on the properties of the root filling material.
IV. APICOECTOMY
Apicoectomy is the surgical resection of the root tip of a tooth and its removal together with the pathological periapical tissues. Accessory root canals and additional apical foramina are also removed in this way, which may occur in the periapical area and may be considered responsible for failure of an endodontic therapy.
ITS INDICATIONS:
➢ Teeth with active periapical inflammation, despite the presence of a satisfactory endodontic therapy.
➢ Teeth with periapical inflammation and unsatisfactory endodontic therapy, which cannot be repeated (Calcified canals, presence of post and cores, breakage of small instruments)
➢ Teeth with periapical inflammation, where completion of endodontic therapy is impossible due to: Foreign bodies driven into periapical tissues, Perforation of root, Fracture at apical third of tooth, Dental anomalies.
If after the apicoectomy, the apex has not been completely sealed, then retrograde filling is required. The purpose of retrograde filling is to obstruct the exit of bacteria and the by-products of non-vital pulp, which remained in the root canal.
CONCLUSION
Root canal treatment of teeth is essentially a prophylactic treatment to clean the tooth from microorganisms and to prevent a perirradicular disease. It should be clear that endodontic procedures should focus not only on prevention of the introduction of new microorganisms into the root canal system but also on the reduction of those located therein. By being familiar with these procedures, the success of the treatment is greatly improved.
CONTRIBUTOR:
Dr. Bryan Anduiza - Writer
Dr. Mary Jean Villanueva - Editor