Often enough I am asked what’s the brand I used, however, although buying branded materials ensures at least the quality of your materials as branded manufacturers do have a reputation to protect, what if you don’t have enough budget in your pocket to buy them? Thus, these are the frequently asked questions often asked but can be answered through the specific characteristic necessary for the material to function properly. By knowing that, you will be able to buy a material whether with brand or not with the right quality you are looking for to do the deed.
Why is there post-operative pain after my restoration when there’s no leak in my composite restoration?
The answer that it is normal to have a post-op sensitivity for 3 days after composite resin is never true. Of course, my answer to this question may not be always this, however, if all probable factors that causes post-op sensitivity never fits to your current case, then, most probably the reason is over etching. The maximum etching time for enamel should not go over 20 seconds while dentin is 15 seconds. If we make a mistake in the time for the enamel, it is often becomes forgivable but for dentin, unfortunately, it will not be the case. We etch in order to prepare the dentinal tubules to be prepared when we placed the bonding agent. Why is that necessary? Because composite resins in general are hydrophobic, so, in order for the composite resin to mesh with dentin, the bonding agent must penetrate at a certain level within the dentinal tubules at least 2-5 microns. If you over etch the dentin, the collagen fibrils will collapse into a thick mat that blocks penetration of the bonding agent and the dentin becomes totally dry on that area, hence, as dentin recovers from its dessication the tooth becomes overtly sensitive. Your composite resin as well is not really properly bonded on your dentin and if your tooth cavity is deep and near the pulp, post-op happens.
SOLUTION: Buy an etchant that has thicker consistency, so, that if you etch first the enamel 5 seconds ahead of time with the dentin, then, it will not over flow to the dentin area before its time to be etched. You CANNOT etch enamel and dentin at the same time, unless, you buy an etchant that has a self-limiting characteristic which means it will stop etching when it reaches a certain depth on the dentinal tubules. The ideal etching time is a total of 20 seconds on both surfaces, 20 seconds for the enamel and 10 seconds for the dentin. And, wash the etchant at least 5-10 seconds. Rinsing time shorter than 5 seconds may not remove residual silica. Moreover, using an actual timer is the best way to solve this problem rather than counting the time on your own. Error on the manner of counting is most often than not the culprit. Such a simple solution yet more often than not we don't practice it.
So, if over etching is a problem, can no-etching bonding agents be used instead?
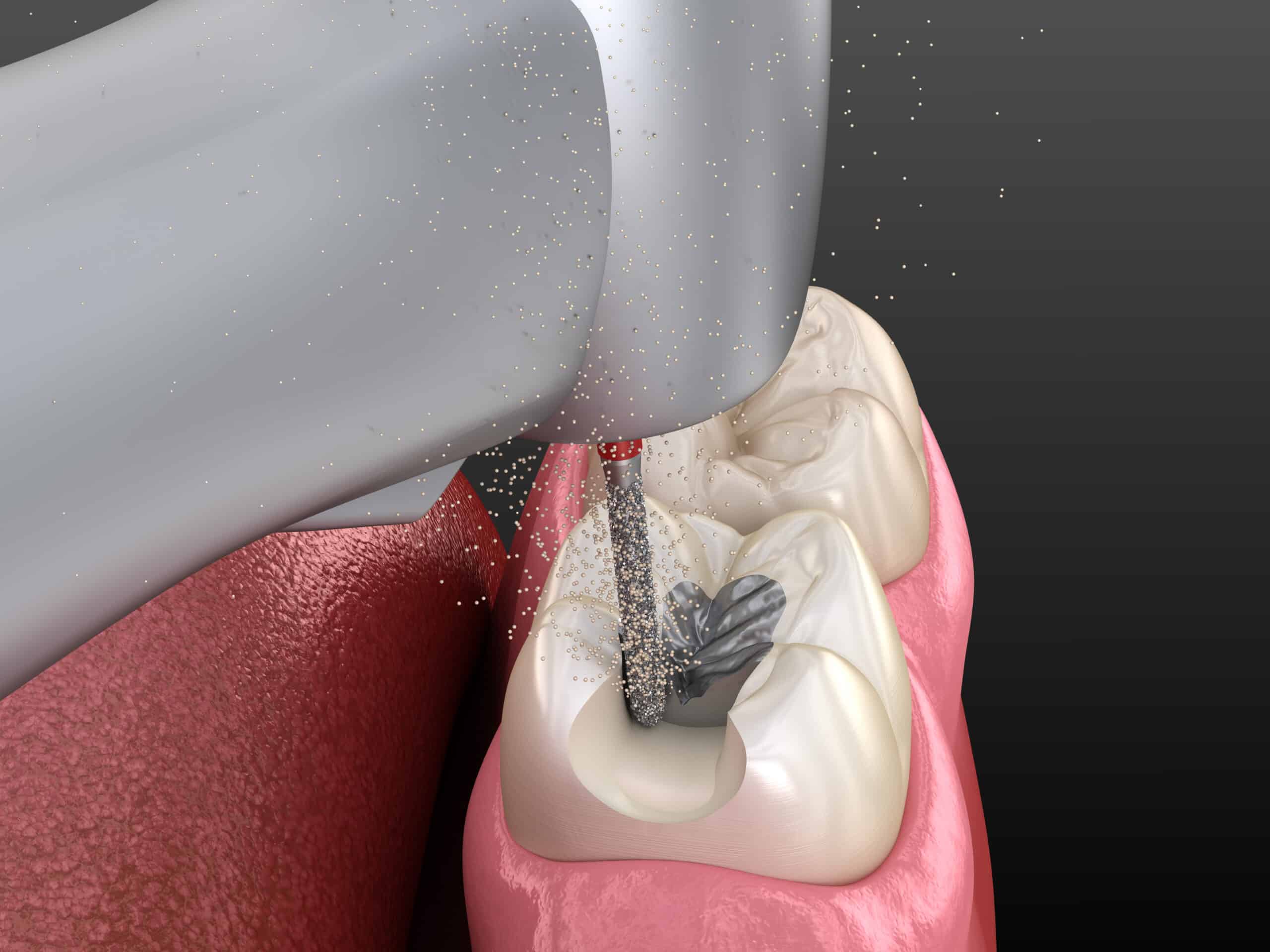
The answer can be yes, depending on the case. No-etching bonding agent normally comes in either 2 or 3 bottles depending on the generation of the bonding agent you are buying. Currently, bonding agents is now up to the 8th generation wherein you can either use total etch or self-etch technique. The premise of no-etching bonding agent is that it has a primer included to replace the etchant. However, there are still studies showing that it may not create the bonding strength necessary to some cases. Ideally, this type of bonding agent is the best choice for restoring teeth of children as it removes the bad taste from the etchant and it can be done quicker than with etching. And, beside comfort and convenience, this is the most important factor to take note, primary teeth should be etched for longer periods (at least 60 seconds), because the surface of the enamel has a prism pattern that is not as well structured and considered aprismatic (without a regular prism pattern), thus, enamel is more resistant to deep resin tag formation. On this cases no-etch bonding is an ideal alternative. Having said that, it is critical that the tooth cavity will not be contaminated by bacteria and residues delivered by the patient’s saliva or blood. Even with the use of etchant this is critical but more so in no-etching bonding agents. If you do use this, I highly recommend rubber dam isolation.
What is the best bonding generation or brand of bonding agent to buy?
Our bonding agent is the glue that meshes our composite resin to our tooth surface. Just imagine when we glue one surface to another such as for example rugby. The surface we need to glue has to be properly prepared. This is the same principle when it comes to bonding composite resin to enamel and dentin surface of our tooth. Both surfaces need to be well prepared, however, no matter how much well-prepared the tooth surfaces maybe if the quality of the bonding agent is not at par to the level of force the tooth will be subjected to during its functions, the bond of our composite with the tooth will break. Unfortunately, unlike, amalgam wherein when it fractures it gets separated with the tooth, thus, more often than not it is only the amalgam that falls out and doesn’t include the part of the tooth, but, when it comes to composite resins the result is catastrophic for the patient’s tooth. Since, composite resins stay in place through adhesive technique, when it breaks or fractures, it goes with the certain part of the tooth structure where it is still bonded. So, unless you are the type who will be happy with this as you will earn more, then, I guess, it is not a problem. But, for those with conscience, then, the solution is to buy a bonding agent with the correct quality and characteristics needed beside placing it properly to the tooth surface during restoration.
SOLUTION: When buying a bonding agent, there 2 critical characteristics you need to look for:
(1) Bonding Strength
(2) Type of Solvent Use.
It doesn’t matter what the brand is but these characteristics of bonding agent you buy are the most important. The average bonding strength needs to be is at least 17-21 MPa (megapascal). Unfortunately, if the bonding agent you use is within the average strength, you have to take note that bonding strength goes down after 24 hours, thus, if the bonding agent you use is only within the average strength, 24 hours later it will be below the average strength required for your composite resin to be bonded to your tooth structure and survive the onslaught of forces it will receive during function. So, the higher the bonding strength, the better chances will your restoration will stay put.
When it comes to solvent, the most ideal is ethyl alcohol. Why? For the resin to penetrate through the water, it must be dissolved in a solvent that can penetrate water and carry the resin with it. The solvents allow the resins to penetrate water on the dentin and in the dentinal tubules, and to penetrate around collagen fibrils and into porosities in the tooth surfaces created by etching. The solvents are primarily acetone, ethanol (ethyl alcohol), or a combination of ethanol and water. In general, the solvent is the largest portion of the bonding agent, making up 60% or more of the material. Acetone is a highly volatile solvent. Its rapid evaporation may require that two or more coats of the bonding resin be applied to ensure adequate sealing of the dentin. (An example of a bonding agent with acetone is Prime & Bond NT [Dentsply].) Ethanol evaporates more slowly, so it may need a longer drying time. (An example of a bonding agent with ethanol is OptiBond Solo Plus [Kerr].). All bottles of bonding agents should be recapped immediately after the material is dispensed, to prevent evaporation of the solvent, which leads to gradual thickening of the resin with less ability to penetrate etched dentin. Unit-dose (single-use) packaging of bonding agents avoids some of these problems associated with bonding agents in bottles, along with infection control issues.
I have bought the bonding agent you suggested but still my restoration breaks or fractures. Why?
There’s no definite answer as to the specific cause of fracture because there’s a lot of them. If we need to figure out the main cause, then, it has to be done on a case to case basis and properly be analyzed. Although, the right materials greatly helps in making your restoration durable, a lot of the fault why it fails is, unfortunately, coming from us. If you believe you are perfect and knows it all, then, good for you. You are the God of all dentists. But, for lesser and realistic dentists, whom I much rather deal with, then, salute to you. In my humble opinion, the best dentists for patients are those who accepts and understands that they are not perfect, that they have limitations and don’t know everything, thus, continually learns from their mistakes and works hard in improving their craft. They are the dentists I highly respect and are writing for because if you know it all, then, there’s no sense for you to waste reading my blogs but instead should be writing it. Anyway, what I discovered, is that the mistake normally comes with the time specified. Like you and everyone else, we are so sure we are counting the time required for us to do the proper application. If you count like me when sometimes I count faster than I should, then, the result will not be the one we want to achieve. In order for bonding to work properly, we need to follow the exact time specified by the manufacturer. It will be different for each manufacturers but what’s critical is we really have to use a timer and not our mind to time the right period of application for agitation, air drying and curing of our bonding agent.
I have bought a composite resin that requires quick curing time, how come sometimes it is not durable?
You have to take note that composite resins that require minimal curing time like 10 seconds need the right light cure unit. The proper and ideal wavelength and light intensity of your light cure unit should be used in order for you to enjoy the 10 second curing time characteristic of the composite resin you bought. This is the same in packable composites as amalgam replacement and that is advertised for skipping the need for layering technique in curing. There are only 2 light cure units that I know as of the moment that do cure whatever proprietary initiators that may have been used by any manufacturer of composites and that is the HIGHER MODEL of Bluephase of Ivoclar-Vivadent and the Valo of Ultradent. There might be new brands now, but, what is critical is that the wavelength of whatever light you may use should be capable of activating the curing of any composite resins that uses whatever proprietary initiators incorporated by its manufacturer. There are some equipment we can’t simply short-change due to cost and one of them is the light cure unit we use, but, that’s only my humble opinion after more than 25 years of practice and training in biochemical compositions of various materials talking, you may know more than I do. If the concern is financial for you to invest in such expensive lights, then, you just have to do multi-layer curing technique wherein you have to cure composites in layers of 1-2 mm thick for 10-20 seconds depending on the quality of the light you use.
I use IRM for temporary cement as evidence-base it works best but I know that it is contra-indicated for composite resins due to its eugenol content. Any advice?
Yes, any temporary cement with eugenol is contra-indicated when the final restoration is composite resin. Eugenol inhibits bonding and curing time of the composite resin. There are temporary cements that are eugenol-free like calcium hydroxide base cements or eugenol-free temporary cement that can be used as an alternative, however, this is only ideal if the temporary filling will be there only up to the maximum of 7-15 days. Why? Because, generally, these temporary cements are water permeable therefore, contamination on the tooth cavity you are observing is high. Thus, not ideal when your treatment for final restoration will require a much longer time or the patient is not known for honoring his/her appointment. On this cases, polycarboxylate cements, resin-based or fiber-glass reinforced temporary or silicone-based filling materials are a much ideal temporarization. However, again, these temporary cements don’t come cheap, so, if cost is the concern, and you really need to use IRM or eugenol-filled temporary cements, then:
(a) You need to completely isolate the tooth such as the use of rubber dam
(b) Remove totally the temporary filling material and make sure it is clean of any trace of it.
(c) Using a cotton pellet, wet it with isopropyl alcohol and wipe the tooth cavity area with it.
(d) Air dry. DO NOT desiccate.
(e) Apply chlorhexidine solution (NOT the MOUTHWASH). Air Dry.
(f) Do the rest of the procedures for composite resin restoration or other treatment such as cementation of post or crown using composite resin as a luting cement.
NOTE: This trick was taught to me in one of the training I attended. But, it is still ideal to use the right temporary material.
Why do you need Chlorhexidine and why can’t I use the chlorhexidine mouthwash?
Chlorhexidine is one of the most effective anti-bacterial solution for several years now along with calcium hydroxide. But, unlike the latter, Chlorhexidine’s method of delivery is either in liquid or gel form. It is not only effective in reducing bacterial colonization but it also increases the bond strength and possible post-op sensitivity caused by one of the factors, the production of MMP (inhibits bonding). Chlorhexidine between 0.02% up to .05% doesn’t affect the bonding strength but actually enhances it because it eliminates Matrix Metalloproteinases (MMP) which our dentin produces after etching. To answer specifically the question is to logically correlate it with something else for easy understanding. Let’s just say when it comes to soap. Our laundry soap is soap, our facial soap is also considered soap. The question is why don’t we not use our laundry soap to our face, since, it is both soap after all, isn’t it? It is because even though they are both soap, each has its own other components that one don’t have than the other do that can be good or bad on its intended function and area of application. It is the same here. Chlorhexidine mouthwash has a component that leaves a thin film in the surface dentin, so, its main function to not hinder in bonding will not occur. In fact, it will become an issue both in restoration and in endo procedures. However, Chlorhexidine mouthwash in my opinion, is the best mouthwash to use as a gargle for your patients during procedures because it assists in killing the bacteria during that time.
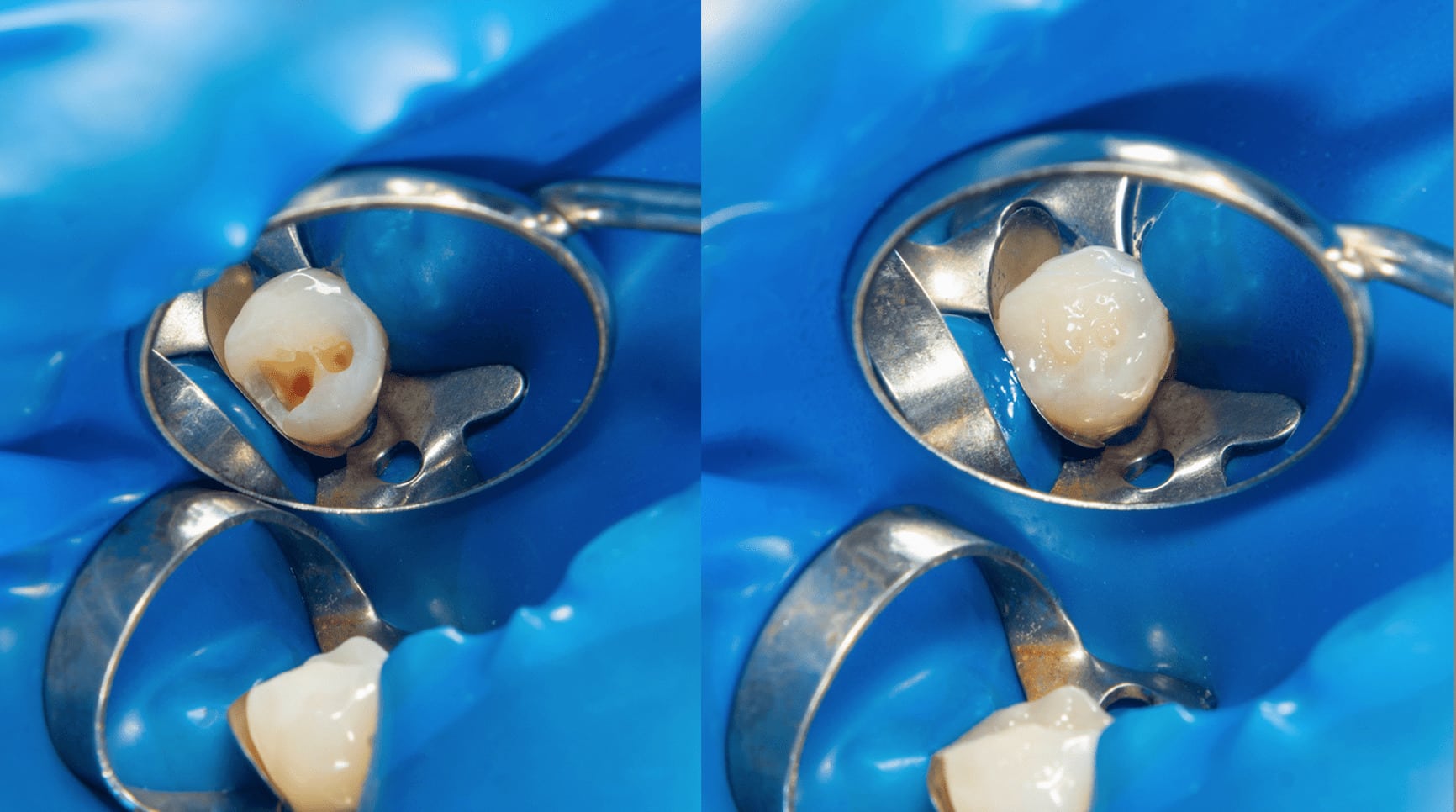
Why is it that when I do restoration, sometimes the margins can be clearly seen after finishing?
There are a variety of factors and I will only mention the most common causes and tips that may result to this error or correct this error, respectively. One of them, is really the manner of shade selection. When shade selection is not done properly, it doesn’t blend well after restoration is done especially for single restoration. Two, is that we over-etch or dry the tooth to become desiccated during shade selection and treatment. So, when the tooth recovers its moisture you will find that you will have a different shade. Three, I find that when I bevel the cavosurface margins, I get best results in blending and I extend the etching a little bit more on the tooth cavity. This allows me to have a bit of the composite outside the cavity to blend well on the remaining tooth surface. Fourth, the manner we carve. Carving and getting the right tooth surface intricacies when we restore helps a lot in blending your restoration with the shade of your natural tooth. And, last, but certainly not the least, we fail to properly mask. Colors are basically produced by light. The manner by which the light can penetrate it or not depends on how we play on the translucency and opacity needed to do an esthetically acceptable restoration. Some cheats on this and just do a one shade restoration. This maybe acceptable most of the time in posterior but not on the anterior restoration and certainly in single tooth restoration. Aesthetic Restoration is similar to applying make-up especially in the area of our eyes, it needs a corrector, a concealer, foundation and then the powder to finish. If you do it that way, most often than not, you will be able to do it right.
What is your opinion on sandwich technique?
Sandwich technique is ideal if we are using 2 different restorative materials that are compatible with each other and can mesh or bond effectively. If your final restoration is one of the hybrid types of composite resins, it is ideally compatible of course with all restorations that contains resins like flowable or fiber-reinforced glass ionomer. Other than that, it will require special bonding materials to make them mesh together to make it durable. Always remember that this technique is generally done in the posteriors, thus, longevity and durability are the most important considerations.
Can we really use expired composites? Does it really lasts for another 6 months after its expiration date?
There are 2 schools of thought on this issue because the answer really is that it depends on how you intend to use it, its storage and the manufacturer. In most manufacturing, the expiration date depends on the regulations of what country the composite was manufactured plus its chemical compositions. In Kits, the manufacturer, normally indicates the expiration date of the product with the least number of shelf-life and this is generally the expiration date of the bonding agent. Thus, even if your bonding agent has expired, your composite resins included on the kit may still be within its “best used before” date. Depending on how you properly handle and store your composites, sometimes it can still be used within what the claim of “can be used” 6 months after the expiration date. However, please do take note that it may not 100% function properly already as like any other products. The expiration date involves safety and the level of the product to perform to its function at 100%. So, if you do indeed use your composite resin after its expiration date, I humbly suggests that it is best to use them as a material for temporarization for veneer, crowns and bridges cases. It is very ideal because your cost is less and you can use this as mock-up for the laboratory and your patient to adjust and see the shape you want the final restoration will be.
[dvk_social_sharing] [et_bloom_inline optin_id="optin_1"]