WHEN IS IT PRUDENT FOR US TO FINALLY DO A MORE RADICAL STEP OF PULPECTOMY VERSUS DOING PULPOTOMY?
Pulpotomy and Pulpectomy are both type of pulp therapy procedures which aims to remove infected or inflamed tissue from the pulpal area of the tooth. The difference between the two is that pulpectomy removes the pulp from the pulp chamber while cleaning and shaping the root canal of the tooth, while pulpotomy focuses solely the removal of coronal portion of the pulp. These two procedures are the preferred treatments for both irreversible pulpitis and symptomatic apical periodontitis especially in children. It is important to be able to distinguish which treatment is needed because it can have a profound impact on the maturation of the tooth.
This post acts as a refresher to what we already know and aims for us to familiarize again the different pulp therapies which can be best used for primary and immature teeth as well as their indications and intended objectives.
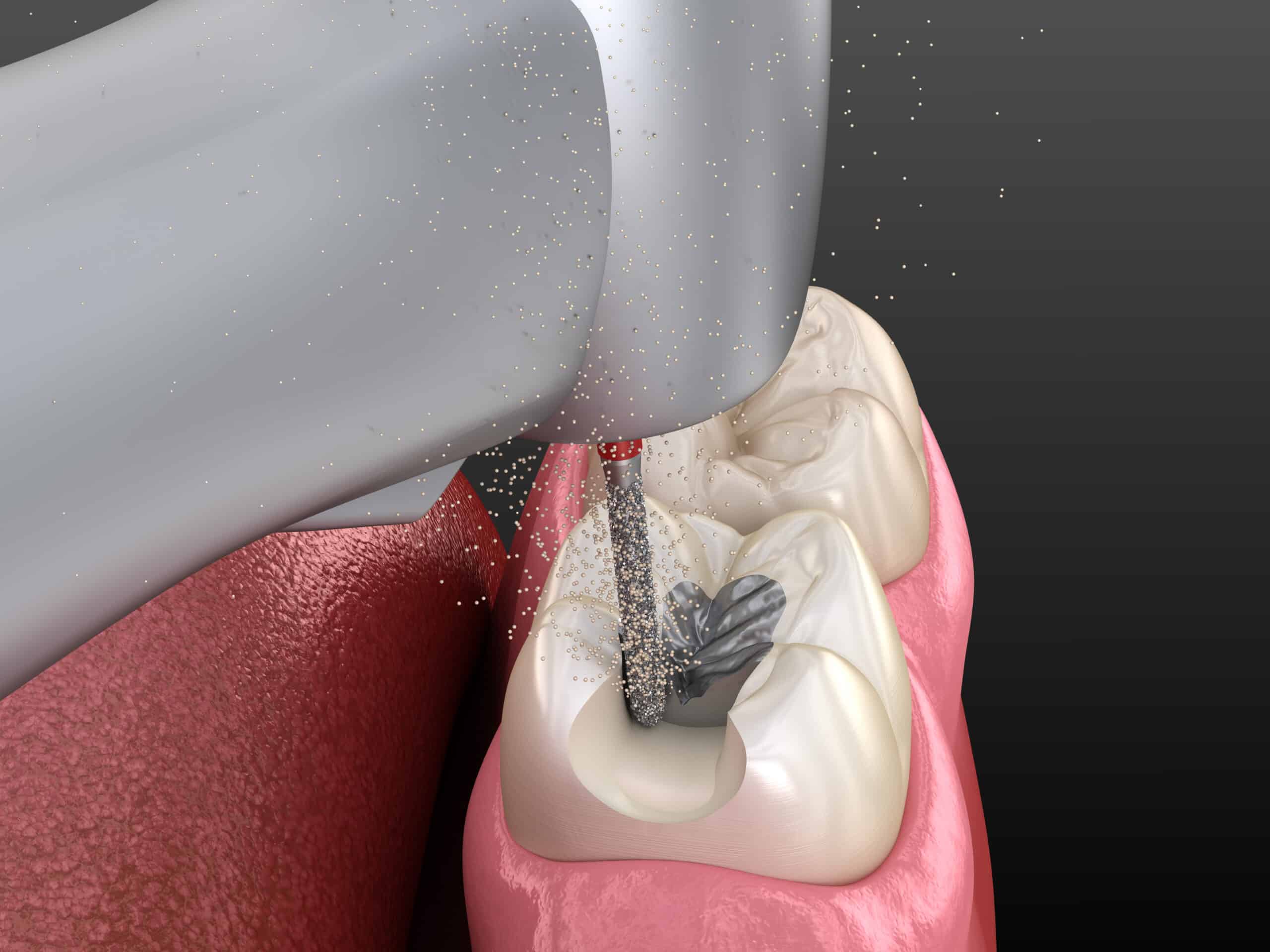
OVERVIEW OF PULPECTOMY
Pulpectomy is a procedure for pulp tissue that is infected by an irreversible pulpitis or necrosis due to caries or trauma. The root canals are debrided and shaped with hand or rotary files. Since instrumentation and irrigation with a solution alone cannot adequately reduce the microbial population in a root canal system, disinfection with irrigants such as sodium hypochlorite and/or chlorhexidine is an important step in assuring optimal bacterial decontamination of the canals. Because it is a potent tissue irritant, sodium hypochlorite must not be extruded beyond the apex. (This can be further avoided with the use of sideport needles).
After the canals are dried, a resorbable material such as non-reinforced zinc/oxide eugenol, iodoform-based paste, or a combination paste of iodoform and calcium hydroxide ( such as Vitapex, Endoflax) is used to fill the canals. The tooth, then, is restored with a restoration that seals the tooth from microleakage.
INDICATIONS:
➢A primary tooth with irreversible pulpitis or necrosis or a tooth treatment planned for pulpotomy in which the radicular pulp exhibits clinical signs of irreversible pulpitis (e.g., excessive hemorrhage that is not controlled with a damp cotton pellet applied for several minutes) or pulp necrosis.
➢Presence of suppuration or purulence of the tooth.
➢The roots that exhibits minimal or no resorption.
Following treatment, the process should resolve in six months, as evidenced by bone deposition in the pre-treatment radiolucent areas, and pre-treatment clinical signs and symptoms within a few weeks. There should be radiographic evidence of successful filling without gross over extension or under filling.
The treatment should permit resorption of the primary tooth root and filling material to permit normal eruption of the succedaneous tooth. There should be no pathologic root resorption or furcation/apical radiolucency.
OVERVIEW OF PULPOTOMY
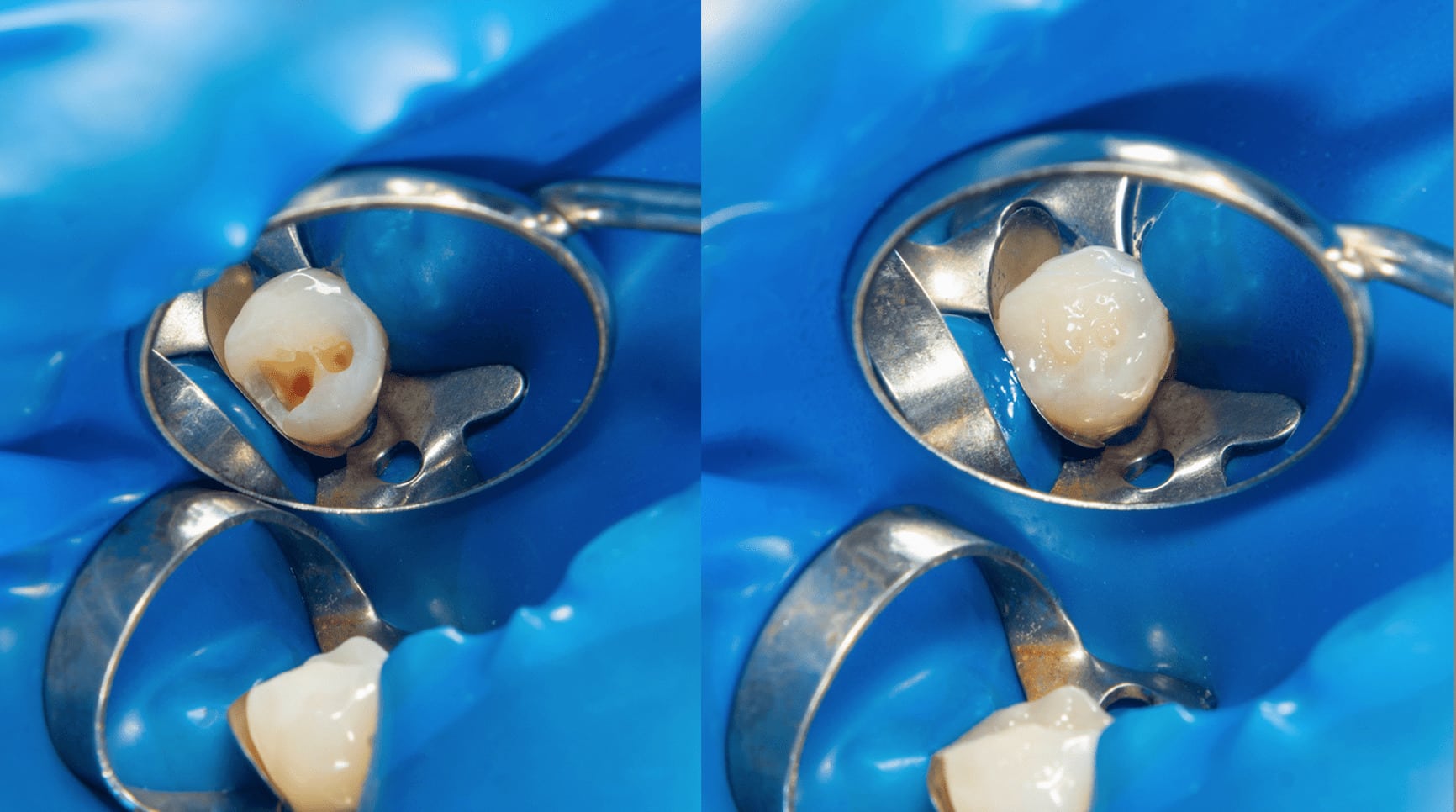
Pulpotomy is a procedure that is performed in a primary tooth with extensive caries but without evidence of radicular pathology when caries removal results in a carious or mechanical pulp exposure.
The coronal pulp is amputated, and the remaining vital radicular pulp tissue surface is treated with a long-term clinically-successful medicament such as Buckley’s Solution of formocresol or ferric sulfate.
Several studies have utilized sodium hypochlorite with comparable results instead of formocresol and ferric sulfite. Hydroxide has been also used, but with less long term success. Mineral Trioxide Aggregate (MTA) is a more recent material used for pulpotomies and creating a breakthrough of a high rate of long term success. Studies shows that MTA performs equal to or better than formocresol or ferric sulfate and may be the preferred pulpotomy agent in the future procedure.
After the coronal pulp chamber is filled with zinc/oxide eugenol or other suitable base, the tooth is restored with a restoration that seals the tooth from microleakage. But the most effective long-term restoration has been shown to be a stainless steel crown. However, stainless steel crown fall down due to the esthetics of the crown. If sufficient supporting enamel remaining, amalgam or composite resin or laser sintered vitrified glass can provide a functional alternative when the primary tooth has a life span of two years or less.
INDICATIONS:
➢Deep caries removal results that in pulp exposure in a primary tooth with a normal pulp or reversible pulpitis or after a traumatic pulp exposure.
➢Radicular tissue should be vital without suppuration, purulence, necrosis, or excessive hemorrhage that cannot be controlled by a damp cotton pellet after several minutes.
➢Cracked tooth syndrome.
The main objective for a successful pulpotomy is that the radicular pulp should remain asymptomatic without adverse clinical signs or symptoms such as sensitivity, pain, or swelling. There should be no harm to the succedaneous tooth. Also there should be no postoperative radiographic evidence of pathologic external root resorption.
Internal root resorption can be limited and stabilized. Internal resorption should be monitored when the affected tooth has perforation that causes loss of supportive bone and/or clinical signs of infection and inflammation through periapical x-rays
ADJUNCTIVE THERAPIES
These are protocols that must be considered in doing pulp therapy to improve prognosis:
1. Adjust the height and contact through occlusal reduction, this can avoid pulpal trauma with vital pulp.
2. Incision and Drainage (I&D): If there is a presence of lesion, this therapy is indicated. Localized, firm or fluctuant soft tissue I/O swelling. Release of fluid pressure, reduction in microbial and inflammatory mediators and prevention of spread of infection to deeper fascial tissues are reasons for employing I&D.
3. Postoperative Antibiotic: Observe for any systemic involvement in all patients. Cases of acute apical abscess with intra or extraoral swelling can cause lymphadenopathy and/or fever which are obvious signs of infection. These are also cues that infection from the pulp and periradicular tissues have spread to deeper and potentially dangerous regions of the body, which must be arrested immediately. Several antibiotics are available that have bactericidal/bacteriostatic properties to endodontic pathogens and present’s positive results
CONCLUSION
We should always remember that the primary objective of any pulp therapy is to maintain the integrity of tooth, the pulp and its supporting tissues. It is the treatment’s objective to maintain the vitality of the pulp of the tooth affected by caries, traumatic injury, or other causes. In preserving the primary tooth we are able to maintain the maxillary growth, aesthetics, mastication, good speech development and prevention of further abnormal habits.
The bottom line is whichever therapy you do decide to apply to your case it should be done quickly and effectively to avoid further pain and infection, thereby, minimizing the development of persistent unbearable pain and formation of periapical pathology that can truly be avoided.
CONTRIBUTOR:
Dr. Bryan Anduiza - Writer
Dr. Mary Jean Villanueva - Editor