How Can We Prevent Mistakes in Prescribing and Dispensing of Prescribed Medicines to Protect Our Patients’ Well-Being?
In any type of procedures, prescription is very important. Prescription acts as a system for the clinician to identify therapeutic alternative to choose what is best for their patients’ needs. It also acts as a guide to enable patients better understand and adhere to their medication regimens and understand the necessity of a medication. Every prescription consists of seven parts: the prescriber’s information, the patient’s information, the recipe (the medication, or Rx), the signatura (the patient instructions or Sig), the dispensing instructions (how much medication to be dispensed to the patient or Disp), the number of refills (or Rf), and the prescriber’s signature (including the PRC number or S2 license#), we will review each of these sections in more detail.
Unfortunately, this benign process that both medical and dental profession have been trained and often do can create sometimes irreparable harm to their patients if not done or provided right. In fact statistics show that all over the world in just a year there are almost 1.3 million cases of injuries from medication related errors due to illegible or unreadable prescription. And, 70 % of this is due to prescription errors. Thus it is important for us clinicians to master the ability to write a prescription properly so it can be delivered right.
On this post, DMD Center will try to provide information that will remind us on how to properly write a prescription and give common sources of prescription errors. Here are the 7 Steps on how to write proper prescription:
PRESCRIBER’S INFORMATION
This information is usually found at the top of the prescription. It generally consists of the prescribing clinician’s name, office address, and contact information (usually the office’s telephone number).
PATIENT’S INFORMATION
Below the prescriber’s information is the patient’s information. This section will include the patient’s full name, age, and date of birth. Sometimes the patient’s home address will be found here, as well. The date the prescription should be specified when it was written.
RECIPE (Rx)
The recipe should include the medication being prescribed, its dose, and its dosage form. For example, if you are prescribing 500 milligram (mg) tablets of Mefenamic Acid, you would write “Mefenamic Acid 500 mg tablets” or “Mefenamic acid 500 mg tabs.”
SIGNATURA (Sig)
After the recipe comes the signatura, which provides the patient with instructions on how to take the medication you are prescribing. This should include information on how much medication to take, how to take it, and how often to take it. For example, if you would like your patient to take one 500 mg tablet of Mefenamic Acid every six hours, you would write “Take 1 tablet by mouth every six hours” or, using abbreviations, “1 tab PO q6h.”
Common Route Abbreviations for Prescription Writing:
- ➢PO (by mouth)
- ➢PR (per rectum)
- ➢IM (intramuscular)
- ➢IV (intravenous)
- ➢ID (intradermal)
- ➢IN (intranasal)
- ➢TP (topical)
- ➢SL (sublingual)
- ➢BUCC (buccal)
- ➢IP (intraperitoneal)
Common Frequent Abbreviations for Prescription Writing:
- ➢daily (no abbreviation)
- ➢every other day (no abbreviation)
- ➢BID/b.i.d. (twice a day)
- ➢TID/t.id. (three times a day)
- ➢QID/q.i.d. (four times a day)
- ➢QHS (every bedtime)
- ➢Q4h (every 4 hours)
- ➢Q4-6h (every 4 to 6 hours)
- ➢QWK (every week)
For as needed or pro re nata (PRN) prescriptions, you should indicate that the prescription is PRN and describe the conditions under which your patient can take the prescribed medication. Writing your prescription as a PRN order essentially gives the patient the option to take the medication when he or she needs it.
Example: Let’s say that you would like your patient to be able to take one 500 mg tablet of Mefenamic Acid every six hours when he or she has a headache. In that case, your instructions would read “Take 1 tablet by mouth every six hours as needed for a headache” or “1 tab PO q6h prn headache.”
DISPENSING INSTRUCTION (Disp)
Next comes the dispensing instructions, which let the pharmacist know how much medication you would like your patient to receive. You should include the amount of medication you would like to be dispensed and the form it should be released in. You should also make sure to write out any numbers you use here to minimize the risk of a medication error. For our Mefenamic Acid example, if you would like your patient to receive a one week supply (or 28 tablets) of the medication, you would write “28 (twenty-eight) tablets” or “28 (twenty-eight) tabs.”
NUMBER OF REFILLS (Rf)
After the dispensing instructions, specify how many times you would like your patient to be able to use this prescription to refill his or her medication. Be sure to again write out any numbers you use. If you do not want to prescribe any refills, write “zero refills.” For our hypothetical Mefenamic Acid example, if you are prescribing one refill, you would write “1 (one) refill.”
PRESCRIBER’S SIGNATURE
At the bottom of the prescription, you should sign your name. Oftentimes, the (NPI) will be included in this section. For controlled substances, the prescriber’s Schedule 2 license Number will also be included.
Problems Encountered During Prescription:
First, if you are writing your prescription, make sure that it is legible. Illegible prescriptions can be a source of problems for patients, pharmacists, and other health care personnel and can increase the risk of medication errors. No matter how busy you are, it is always better to spend a few seconds slowly writing out legible prescription than risking your patient’s safety and health.
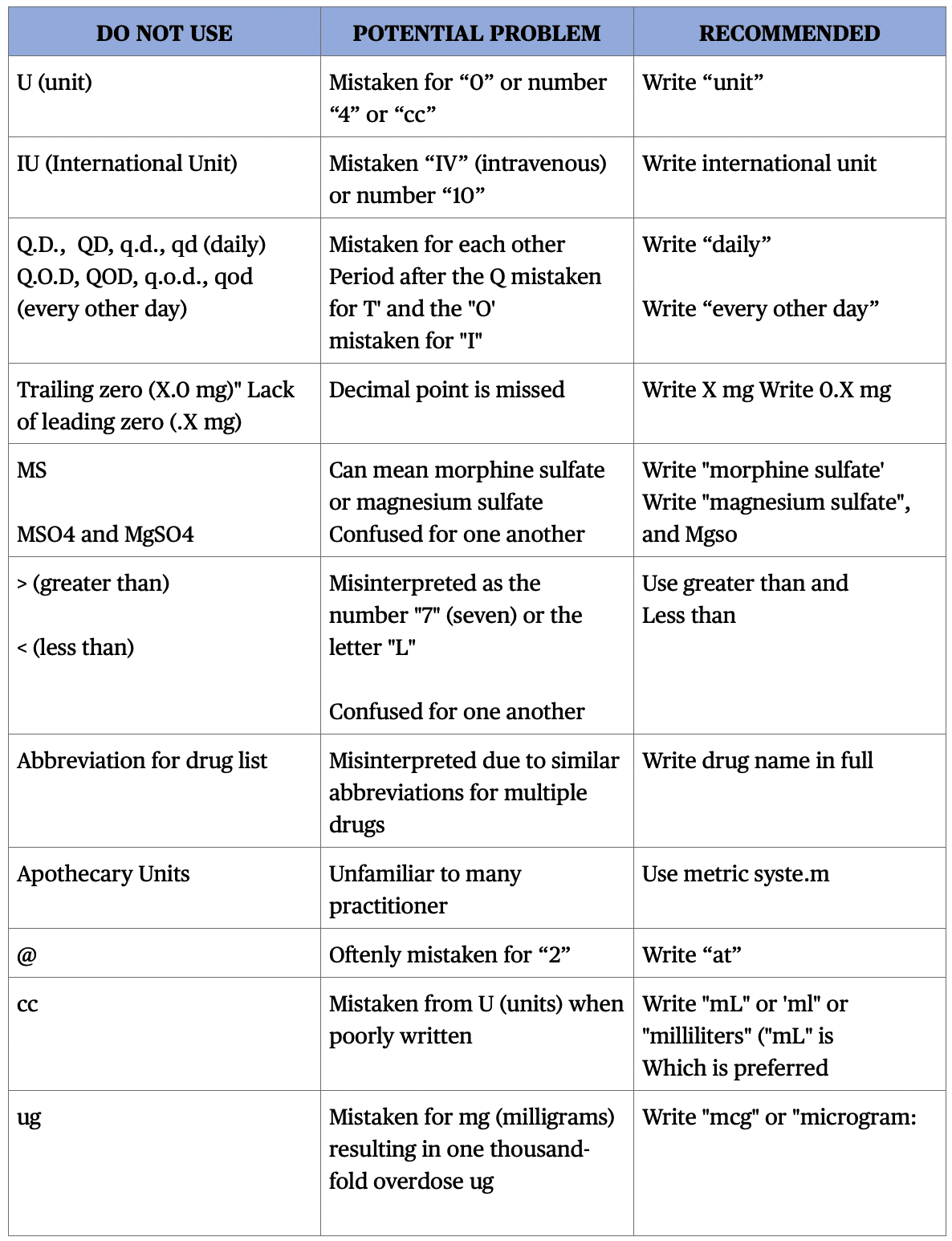
Second, when using abbreviations. While abbreviations are commonly used in medicine, you should keep in mind that the risk of a medication error is increased when abbreviations are ambiguous or used incorrectly. So if you choose to use abbreviations in your prescriptions, be sure to only use well-known ones if you are unsure whether or not you should use an abbreviation, just spend the extra few seconds to write out your directions completely.
Here is a list of what should be:
CONCLUSION
In conclusion, it is important to write legible and be aware of the do not use list when prescribing. Problems in prescription are easy to be avoided but has a great consequence when you create mistakes. By being aware of this we become more vigilant and aware of what our patients' needs and ensure their safety.
Contributor:
Dr. Bryan Anduiza - Writer
Dr. Jean Villanueva - Editor
[dvk_social_sharing] [et_bloom_inline optin_id="optin_1"]