IS LASER TECHNOLOGY SOMETHING WORTH TO INVEST IN OUR DENTAL PRACTICE?
One of the dental methods that we can use to make some of our dental procedures easier is the technology that became commercially available in dentistry in 1989, the LASER. LASER stands for Light Amplification by Stimulated Emission of Radiation. This is a device that produces light by optical amplification based on electromagnetic radiation stimulation. The light it emits is a narrow, low divergent beam that is known as spatially coherent feature. This has been used in other industries prior to its introduction to dentistry such as in the field of medicine for surgery and various skin treatments or even in consumer devices as banal as barcode scanners and printers. In dentistry, its introduction is intended to improve our treatment to be highly focus on a specific area we are treating so we can avoid damaging surrounding tissues. One of the very first laser used in dental industry is the ND-YAG (Neodymium-doped Yttrium Aluminium Garnet), the CO₂ laser is 1994, the laser welder in 1996 and ER-YAG (Erbium-doped Yttrium Aluminium Garnet) laser in 1998. In soft tissue, the lasers generally used is CO₂ and ND-YAG while for hard tissues, ER-YAG and Excimer.
Let's delve into certain basics about LASER, so, we can understand it even better and be able to assess if this technology is for us to use in our dental practice.
MECHANISM OF ACTION
1. Laser Physics
- The stimulated emission is a phenomenon that occurs within the active medium. The active media can be solid state, gas or semi conductor.
Photo is Courtesy of Dental Compare Website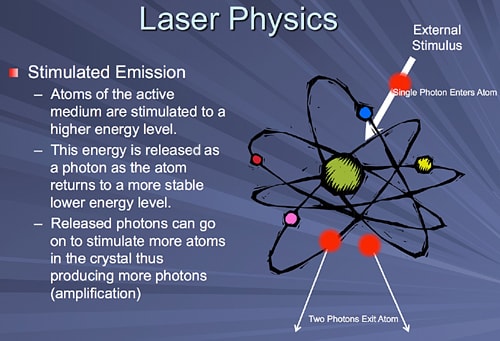
➢The energy that it produces controlled by the operator has a measuring unit in millijoule (mJ)
➢Its power is measured in Watts (W) and 1 watt is equals to 1 Joule/second. These are the watts displayed on the machines' control panels. A laser beam can be emitted either as a continuous beam or in a pulsed fashion.
➢The pulse rate per second is measured in Hertz (Hz).
➢The wattage displayed on the laser unit is a product of the Millijoule (energy) per pulse times the number of pulses per second (hertz).
➢Peak Power refers to the power level in each individual laser pulse and this measurement is not visible to the operator, yet it is the most important variable dictating how the laser beam will interact with the target tissue.
To understand the peak power, one can think of a rubber band around a wrist as an analogy. If the rubber band is lifted three inches, it will have a fixed amount of energy in it. Now if the rubber band is slowly returned to the wrist, it will not hurt a bit. If it is let go, the energy is released in a much shorter time and it will sting and make a popping sound. Yet the actual energy expended is identical. Hard tissue dental lasers can have peak powers in the thousands of watts, and these short burst of extreme power allow for the efficient cutting of enamel, dentin and bone.
(a) Gated Wave - is usually created with a shutter that blocks the laser beam from reaching the handpiece and target tissue at varying speeds. This pulse form is sometimes referred to as "chopped." The laser is on constantly but the shutter device blocks the light from transmitting. "Superpulsed" lasers are a form of gated lasers with extremely short pulse durations.
(b) Free Running Pulsed - is not on constantly but emit photons in powerful bursts of energy measured in millionths of seconds
The best way to understand this Pulsed Laser Modes is when a flashlight is turned on it is in continuous wave mode, moving one's hand back and forth across the beam is gated wave mode, and turning it on and off repeatedly is free running pulsed mode. Each of these temporal emission modes has important characteristics when the laser energy interacts with tissues that need to be understood well by the practitioner.
2. Design of Laser Medium - The components of a typical laser are the following:
(a) Gain Medium
(b) Laser Pumping Energy
(c) High Reflector
(d) Output Coupler
(e) Laser Beam
Photo is Courtesy of Dental Compare Website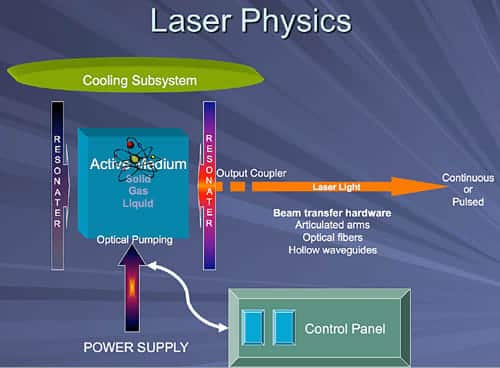
3. Tissue-Laser Interaction - depending on the optical properties of the specific tissue being treated, laser light can have 4 different interactions with the said tissue:
(a) Absorption - Specific molecules in the tissue known as chromophores absorb the photons. The light energy is then converted into other forms of energy to perform work.1
(b) Transmission - The laser energy can pass through superficial tissues to interact with deeper areas. Retinal surgery is an example; the laser passes through the lens to treat the retina. The deeper penetration seen with Nd:YAG and diode lasers is an example of tissue transmission as well.1
(c) Reflection - The laser beam bounces off the surface with no penetration or interaction at all. Reflection is usually an undesired effect, but a useful example of reflection is found when Erbium lasers reflect off titanium allowing for safe trimming of gingiva around implant abutments.1
(d) Scattering - Once the laser energy enters the target tissue it will scatter in various directions. This phenomenon is usually not helpful, but can help with certain wavelengths biostimulative properties.1
Photo is Courtesy of Dental Compare Website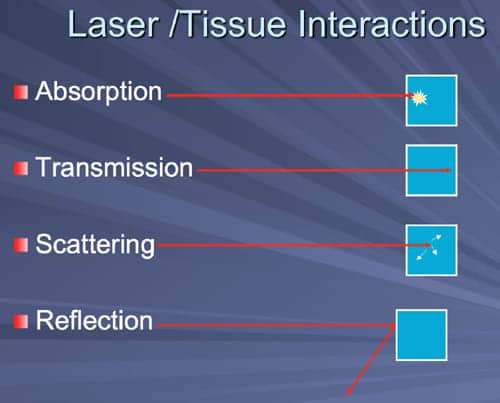
➢Laser technology uses the principle of selective photothermolysis which means the laser targets the different chromophores in the skin which selectively absorb the light energy (laser) as heat and yield the desired result. It is important to take note that there are different results as temperature changes.
1. 37° - Normal
2. Between 45°-50°
➢there’s vasodilation, reduction of enzyme activity, hyperthermia and cell immobility
3. Between 60°- 80°
➢there’s and increase of blood viscosity resulting to coagulation
4. 100°
➢the tissue shrinks and gets dehydrated resulting to vaporisation, carbonisation and irreversible cell death
5. 300°
➢Melting
USAGE TO DENTISTRY
1. Diagnostic Tool
- ➢Detection of pulp vitality
- ➢Doppler Flowmetry
- ➢Laser fluorescence wherein it can do caries and bacterial detection as well as cause dysplastic changes in cancer diagnosis.
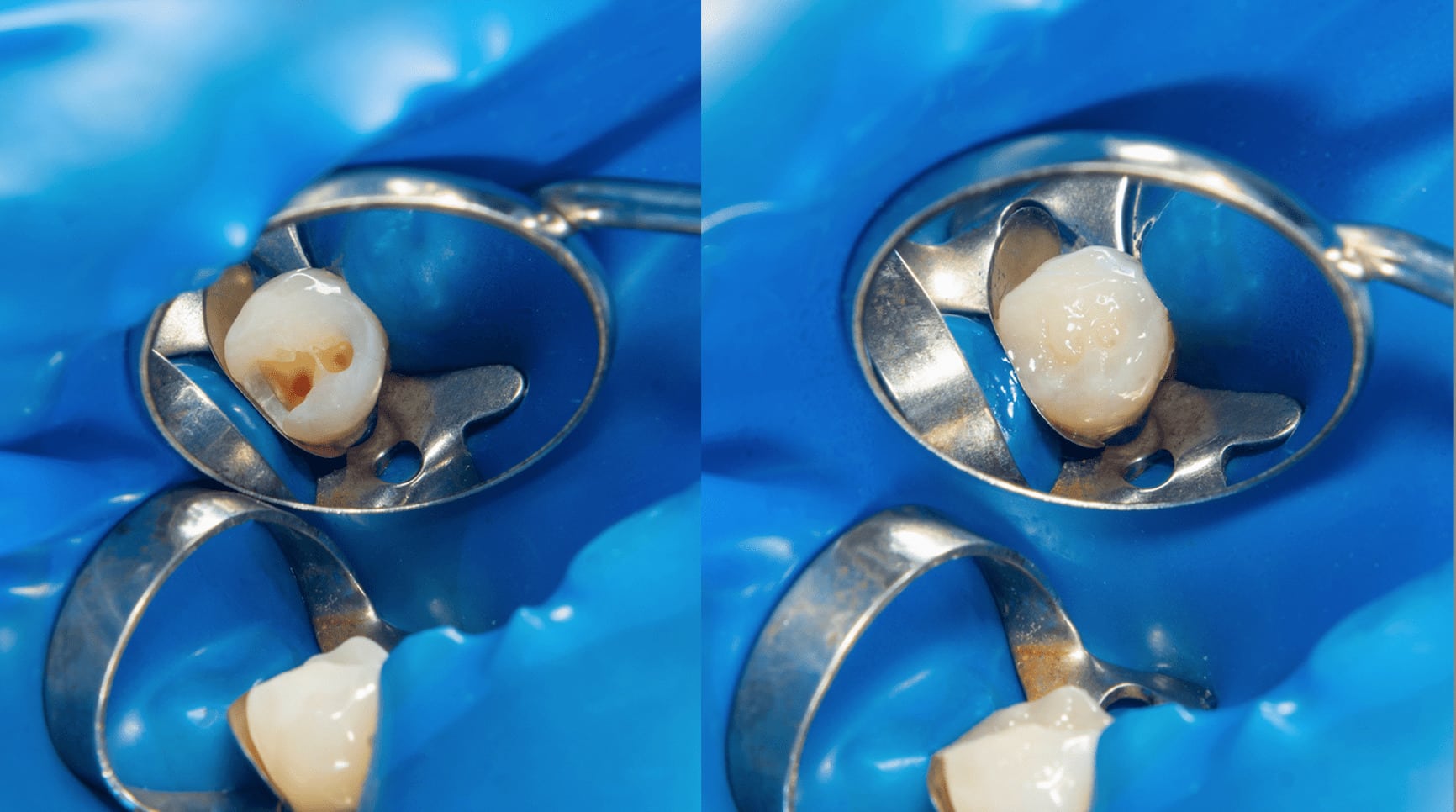
2. Application on Hard Tissues
- ➢Removal of Caries and Cavity Preparation
- ➢Crown Lengthening through Bone Re-Contouring
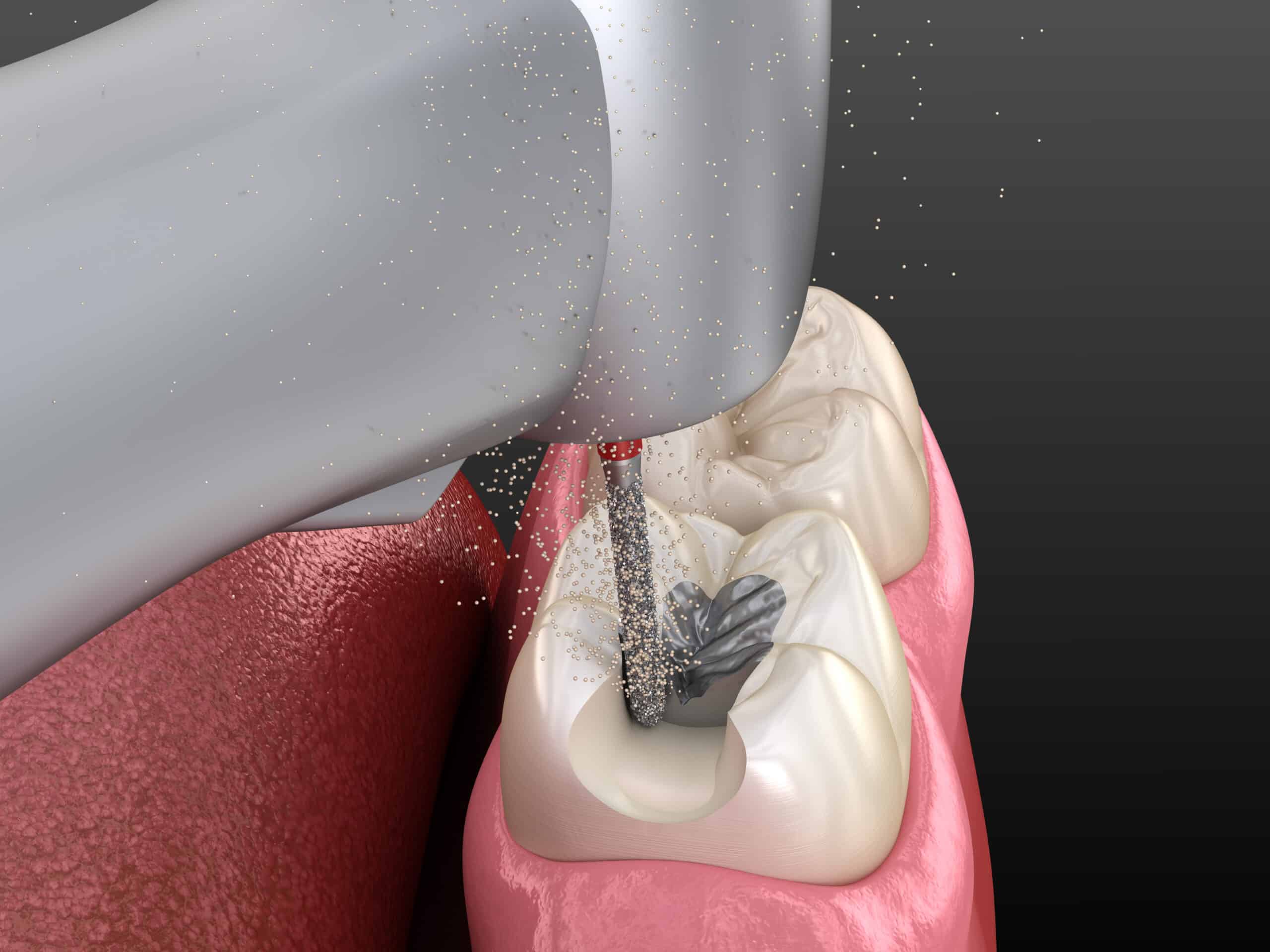
- ➢Root Canal Preparation, Canal Sterilization and Apicoectomy
- ➢Do Etching
- ➢To Increase Caries Resistance
3. Application on Soft Tissues
- ➢Soft Tissue Curettage and Per-Apical Surgery Assistance
- ➢Bacterial Decontamination
- ➢Gingivectomy and Gingivoplasty
- ➢Gingival Retraction for Impression
- ➢Implant Exposure
- ➢Biopsy Incision and Excision
- ➢Aphthous Ulcer Treatment and Oral Lesion Therapy
- ➢Coagulation and Hemostasis
- ➢Tissue Fusion - Suture replacement
- ➢Flap Surgery Assistance
- ➢Granulation Tissue Removal
- ➢Pulp Capping, Pulpotomy and Pulpectomy
- ➢Operculectomy and Vestibuloplasty
- ➢Incisions
- ➢Abscess Drainage
- ➢Hyperplastic and Fibromatous Tissue Removal
4. Laser-Induced Analgesia
5. Laser Activation - used to cure composite resins and bleaching agent activator
6. Miscellaneous Functions such as the following:
- ➢Root Canal Filling Material and Fractured Instrument Removal
- ➢Gutta-Percha Softener
- ➢Drying Root Canal
ADVANTAGES OF LASER USAGE
1. On certain cases, it reduces the use of anaesthesia.
2. Reduces patient’s anxiety with the need of use of dental drills.
3. Minimizes bleeding and swelling.
4. Decrease chances of bacterial infections
5. Minimally invasive as it reduces the need for more tooth reduction.
DISADVANTAGES OF LASER USAGE
1. Limitation on restoring teeth that has current restorative filling materials.
2. Limitation on many of the commonly performed dental procedures such as interproximal and large cavities.
3. Traditional dental drills may still be needed on certain procedural steps such bite adjustment and finishing and polishing of restorative materials.
4. Still requires anaesthesia.
5. Its cost.
PRECAUTIONS
1. Safety eyewear protection for both dentist, patient and dental assistant.
2. Avoidance of looking at the laser beam directly.
3. Always point the laser handpick only at the area to be treated.
4. Never use laser in the presence of inflammable dental materials such as anesthetics.
5. The finer optic cable must not be step on or bend.
6. Make sure the laser machine is positioned in a stable area during operation.
CONCLUSION
There are many benefits that laser can bring into our procedures especially to the post-operative benefits to our patients in terms of time of healing and less experience of pain or discomfort. However, it must be said that using this technology requires one to fully understand its functionality, thus, the need for training is a MUST. I believe that training not only enables us in maximizing its usage to provide value in our investment but, at the end of the day, ensures our patients’ safety.
CONTRIBUTOR:
Dr. Mary Jean Villanueva - Writer | Editor
REFERENCES
1. Lasers in Dentistry: Minimally Invasive Instruments for the Modern Practice Stimulated Emission by
Steven R. Pohlhaus, DDS
2. Dinesh Raj Lecture, Klink Pergigian Besar Kota Bharu