WHY DO YOU NEED TO CARE?
The most common misunderstanding when we practice infection control in our dental practice is that we think we do it primarily for our patients’ protection. The truth of the matter is the practice of doing proper infection control is for our own protection and the people who work for us. We are more the most vulnerable in acquiring contagious and infectious diseases as we are exposed at least 8 hours a day, 5-6 days a week and 4 weeks in a month. Our patients only stay in our clinic in a matter of 30 minutes minimum or 4 hours maximum for extensive procedures. Thus, the practice of infection control is for us and our well-being. So, let’s tackle the basic infection preventive recommendations prepared by the Centers for Disease Control and Prevention.
A BROADER PERSPECTIVE
Infection control may be classified as a feature of health-care practice which involves processing used instruments for re-use in clinical practice, controlling the spread of cross-contamination in the dental settings by nullifying or limiting the exposure to pathogenic microorganisms, increasing the resistance to infectious diseases and effective waste management
With the resurgence of pathogens and infections, the threat of cross-infection in dental practice has been magnified. Such as the transmission of dental infection can occur through infected air droplets, blood, saliva, and instruments contaminated with secretions. Persons who seek dental care could be the carriers of certain infectious diseases, without knowing about their physical conditions. In addition, some infectious diseases have a prolonged incubation period or post-infection “window period” during which antibodies can’t be detected.
Cross-infection in dentistry can occur through many pathogenic organisms found in the oral cavity and respiratory tract. Examples of these organisms are cytomegalovirus (CMV), Hepatitis C Virus (HCV), Hepatitis B Virus (HBV), herpes simplex virus (HSV types 1 and 2), HIV/AIDS, Mycobacterium tuberculosis, staphylococci, streptococci, and other viruses and bacteria. Furthermore, nowadays we are living in an era of eco-epidemiology, with global emergence and re-emergence of many communicable diseases. Emerging agents as Ebola, Polio, Middle East Respiratory Syndrome-Corona Virus (MERS-CoV), H1N1 and H5N1 and others can be also transmitted during dental practice.
With the alarming increase rate of bloodborne infections such as HIV/AIDS, HCV, HBV, and other emerging bloodborne diseases represent the main risks transmission of infection in dental practice. Exposure to blood and body fluids need great concerns from both dental care providers and patients.
12 BASIC RECOMMENDATIONS
I. Distinguishing Re-Usable and Consumables.
Dental professionals should be aware of which devices are reusable and non-reusable. All of these should be disposed properly once their usage has been consumed. Dental instruments, devices, and equipment are profiled in different categories based on their potential risk for infection together with their purpose, such as critical, semi-critical and noncritical.
- Critical items should always be sterilized with heat.
- Semi-critical items should also be sterilized with heat. If it isn’t heat-tolerant, it should be replaced with a heat-tolerant material. Otherwise, it should not be reused.
- Noncritical items should be cleaned followed by disinfection using an EPA-registered hospital disinfectant.
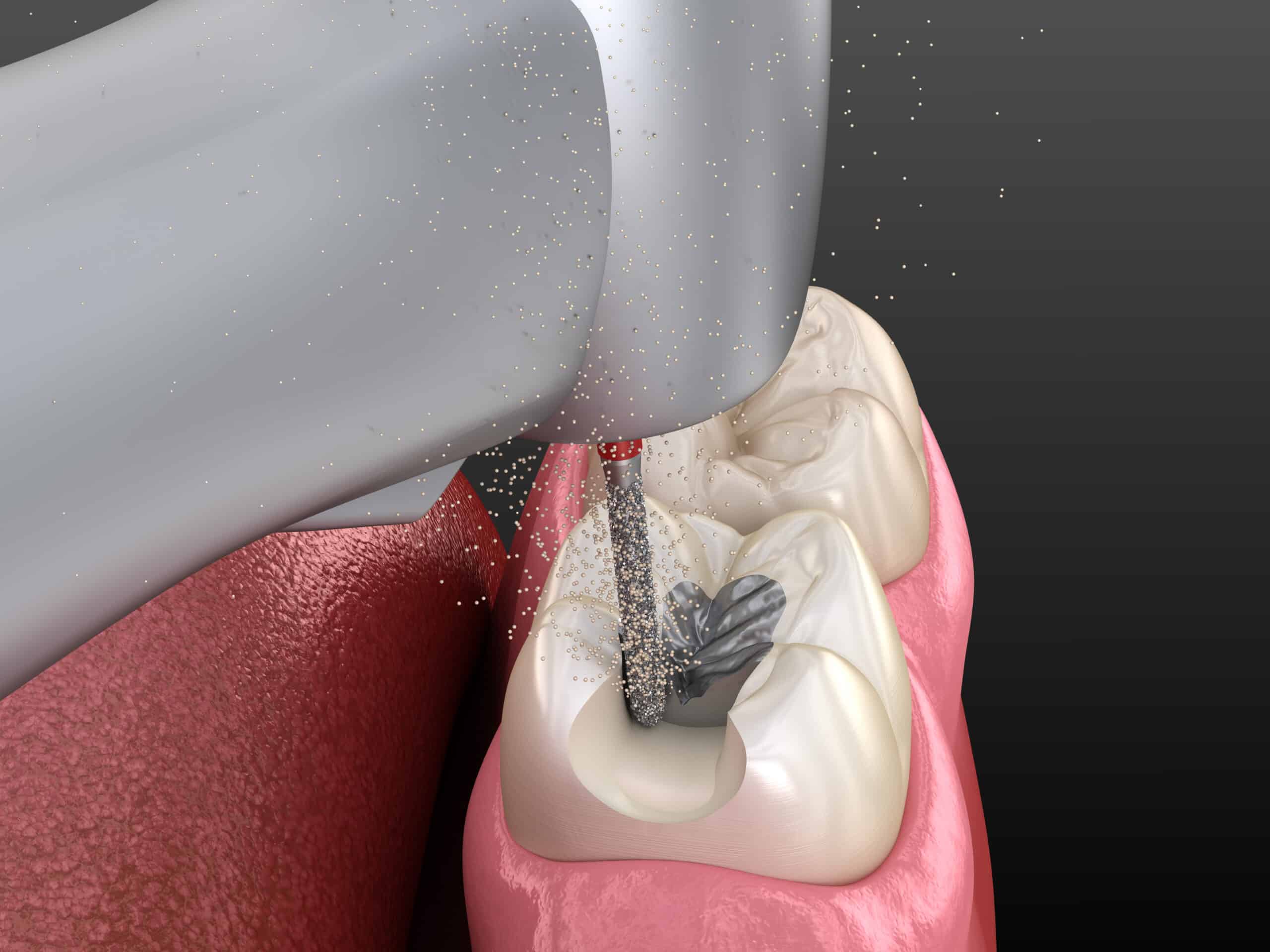
CLEANING & DISINFECTION
STERILIZATION - SATURATED STEAM UNDER PRESSURE
II. Handling Must Follows Manufacturer's Instructions.
All dental equipment should be cleaned and reprocessed as stated by the manufacturer. If there aren’t any instructions provided, the device isn’t appropriate for multi-patient use.
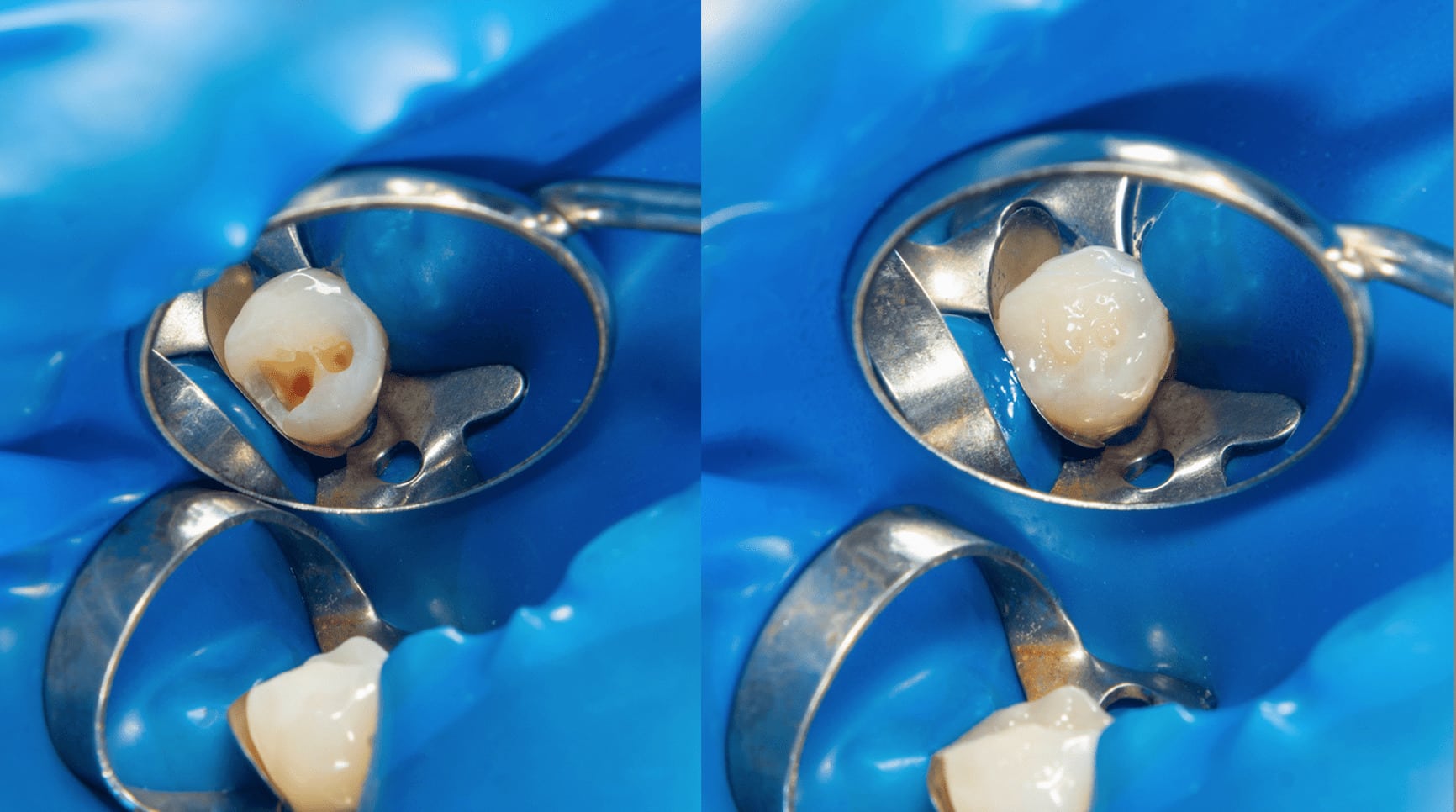
III. Certain Conditions Requires Immediate Cleaning
Dental materials such as cement, composites and glass ionomer should be immediately cleaned from the dental instruments after use because these materials have a tendency to set and harden. Once that happens, these cannot be removed by simply using automated cleaning equipment.
IV. Precision In Measurement
Infection control works base on 2 factors, the duration of time of exposure and the proper volume or measurement used in exposure. Be precise in using the correct amount of product. For example, one packet of Biosonic Enzymatic Ultrasonic Cleaner makes one liter of solution, and if you are using a two-liter ultrasonic tank, you should make use of two packets.
V. Know Its Function and Purpose
Make sure that dental products are being used according to their true purpose. For example, in ultrasonic cleaner always use a solution with neutral PH or alkaline PH. The solution must at least have enzymes such as amylase and protease for effective cleaning. Never use glutaraldehyde or disinfecting solutions as a holding solution or for an ultrasonic.
VI. Proper Handling of Instruments & Other Hazardous Materials
Do not reach for trays or containers that may have unseen sharp instruments. Sharp objects such as disposable syringes, needles, scalpel blades should be placed in non-puncturable containers. These containers should be placed in the nearest possible area where these instruments are being used.
VII. Use of Proper Containers
During cleaning and disinfection process, use a strainer or an instrument cassette for loose or sharp materials. This helps the instruments being cleaned have greater longevity and will significantly reduce any risks of injury while cleaning.
DENTAL CASSETTES
DENTAL STRAINERS FOR BURS AND SHARP INSTRUMENTS
VIII. The Right Conditions
Ensure that all instruments are fully dry prior to wrapping and sterilization. Sterilizers only remove the same amount of moisture they put on the instruments. So if instruments are placed in wet, they come out wet. Wetness easily attracts bacteria, which increases the risk of contamination.
IX. The Correct Packaging
Do not overfill your sterilization pouch with instruments. Always pack them according to the manufacturer’s instructions. Over packing is the usual cause of failed sterilizations. Sterilizers will take more time to reach the optimal temperature, and since the instruments are packed too closely, the correct amount of sterilizing agent will not be distributed properly.
PROPER AUTOCLAVE CONDITIONS - CLASS B STERILIZER
X. Use of Proper Attire
When cleaning instruments, always wear the proper attire — puncture-resistant utility gloves, protective eyewear, mask, and clinical gown. Make use of long-handled brushes to further prevent injury.
XI. Manuals Must Be Readily Available
The manufacturer’s instructions should be made readily available within the reprocessing area. All instructions should be maintained by each personnel responsible for processing the instruments.
XII. Inspection is a Must
Always inspect the instruments after cleaning. Look for residual debris and re-clean them if necessary. Check for worn out or dull instruments. Use appropriate and adequate lighting while checking and utilize a magnifying glass if deemed needed.
IN CONCLUSION
Infection control nowadays is highly crucial in medical and dental practices in order to lessen the risk of any disease from potentially spreading and prevent the most common health care complications. It promotes a sanitized and safe environment for everyone who enters any clinical setting. Failure to contain an infection from spreading poses a great threat to the well-being of medical and dental professionals, their patients and, in a larger scope, the public. There are general precautions for infection control required to be performed during clinical practice in a patient set up.
Contributors:
Dr. Bryan Anduiza
Dr. Jean Galindez
Credits on Image:
https://www.juniordentist.com
https://www.sonicsonline.com
https://www.adwdiabetes.com
https://www.safcodental.com
https://fr-ca.ecolab.com
https://appadvice.com