IS IT SAFE TO TREAT RECOVERED COVID-19 PATIENTS? WHAT ARE THE PROTOCOLS TO KEEP US SAFE?
The initial outbreak of the novel coronavirus has successfully shutdown almost 8,000 dental practices in the Philippines. When the Philippine government declared the resumption of health services, dental organizations are in discussion of how can they provide a safe oral healthcare at the midst of this pandemic. As we all know a lot of patients have been delayed of having their procedures, their treatments placed on hold, and, for some, even long overdue. Because of this situation, there are risks that our patients have to bear when their treatments are prolonged and delayed. Unfortunately, there are still a lot of unknowns and inconclusive facts about this CoVid-19 virus especially that it already mutated into different variants. Thus, one of the concerns is our ability to continually protect ourselves when we practice especially not only with dealing possible CoVid positive patients, but, those recovered from it, but, maybe in relapse.
Before we delve into it, first, let's discuss briefly the important points on what researchers have provided us about CoVid-19 virus in relation to this topic.
One, controlling the spread of SARS-CoV-2 requires a different approach from its related virus family. COVID-19’s incubation period can range from 2-14 days and, even if the virus is known to be highly transmissible when patients are most symptomatic, transmission can still occur even before any symptoms manifest.
Second, we need to deal with the situation of possibility of relapse and reinfection. So, for clarity sake, let's define the epidemiological meaning of these 2 conditions. Relapse is when the virus gets treated, the symptoms have disappeared and the patient gets a negative result after test, but, unfortunately, it turns out that the negative result is not because the patient has fully recovered. It’s actually because the volume number of the virus has significantly reduced that any CoVid tests can’t detect its presence anymore. This generally occurs 5-10 days after patients get discharged from the hospital. Thus, the patient can still be contagious if the CoVid virus regenerates due to patient's still low immunity, and, result to relapse. Reinfection, on the other hand, means that the patient has truly fully recovered, yet, the patient can still contract it again after a certain time and still not totally immune from CoVid-19. It is important to state that there's no definitive data as of the moment that concludes reinfection can still occur for recovered CoVid patients after several months or years.
Third, what can a recovered CoVid-19 patient responsibly do if the patient sense a relapse or possibility of "reinfection" is to consult an infectious disease doctor and do isolation again before and during this medical evaluation, particularly, if symptoms returns after close contact with an infected person. It is important to take note, that a CoVid patient should take CoVid tests with at least 2 negative results to be safely declared as CoVid-free and has fully recovered.
So, as the CoVid cases went higher, new variants were discovered, research of the nature of the virus was published and notifications of how this virus can exposed us when we do dental procedures, it bears to question now, how can we, as dentists, be able to safely do dental procedures with our patients who recovered from Covid with a possibility of not being fully recovered? This post will discuss the guidelines to address your concerns on handling CoVid recovered patients in order for us to still do our profession without discrimination and at the best of our ability adapting protocols to protect ourselves and our staff from this deadly virus.
EMERGENCY DENTAL CARE ONLY AT A TIME FRAME
CDC recommends that for CoVid recovered patients, only elective dental services can be given until the patients has done isolation for at least another 2 weeks after the patient's recovery or 2 negative results have been produced from a CoVid test from the time of patient's recovery.
RECOMMENDED PROTOCOLS FOR ELECTIVE EMERGENCY CARE
A. Set the operatory tray with clean or sterile supplies and instruments that are necessary only for the dental procedure.
All other supplies and instruments should be properly stored and other fixtures such as drawers and cabinets are covered or placed away from the treatment area to avoid potential contamination. Any fixtures, materials, supplies, and equipment that are not used during the procedure yet exposed on the treatment area must decontaminated or disposed, if necessary.
B. A negative pressure room, if possible, is the ideal treatment area to do your dental emergency care especially if the dental procedure is considered to be an aerosol-generating dental procedure.
C. During a potentially aerosol-generating dental procedure, it is ideal to use a portable HEPA air filtration unit located within the vicinity of the patient's chair, but, not behind the DHCP.
D. The use of exhaust and extra-oral vaccuum may be effective in reducing aerosol inside the treatment.
E. Follow the standard contact and airborne precautionary protocols including hand hygiene practice to the letter.
F. Consider taking extraoral radiographs instead of intraoral (e.g. panoramic radiography) to avoid gag reflex.
G. Limit the number of dental staff present during the procedure to only those essential for patient care and procedural support. In terms of patient's companion, it should be limited to what and who is necessary to be there.
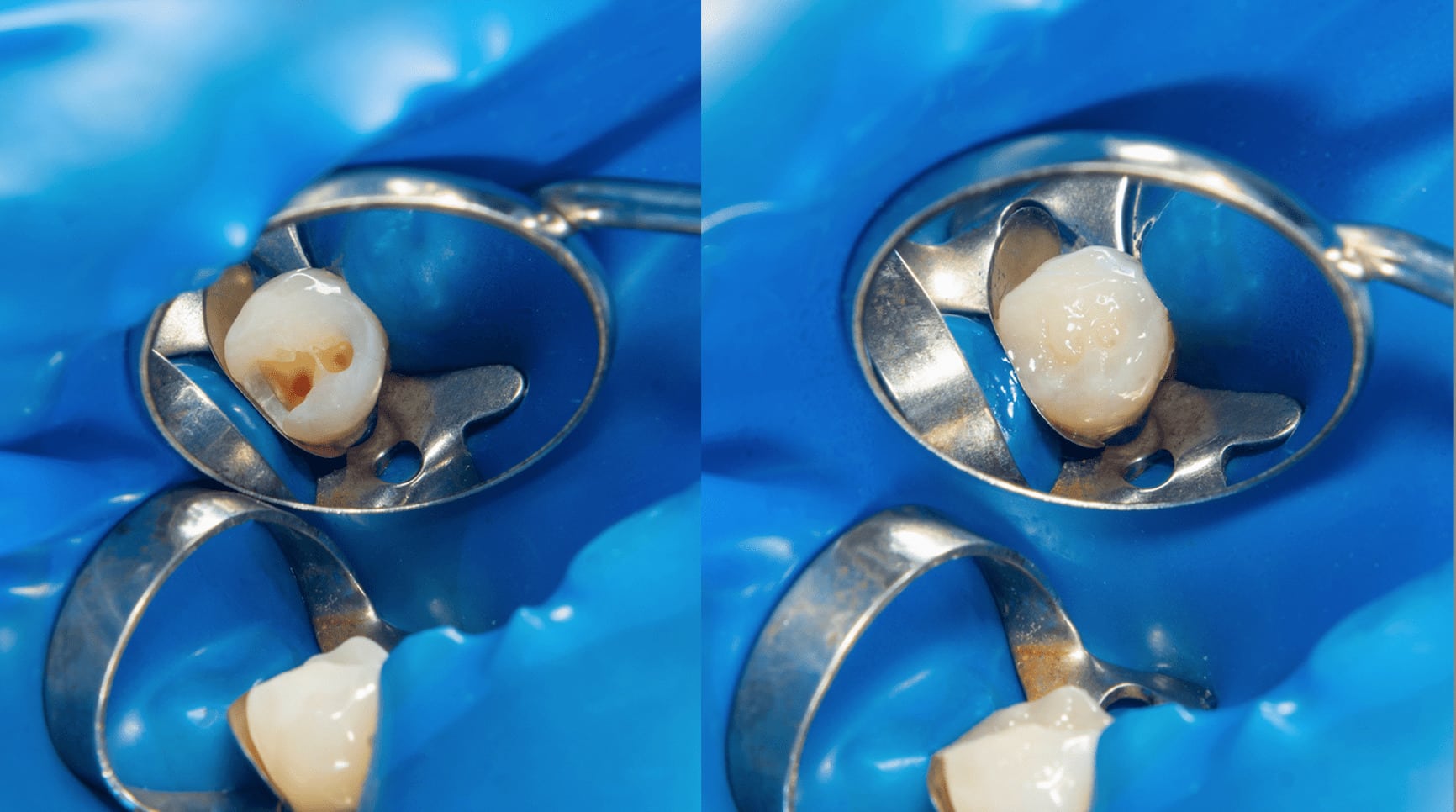
H. Use a dental hand-piece with antiretraction function, four-handed dentistry, high evacuation suction and rubber dams to minimize droplet splatter and aerosol generation.
I. Minimize the use of ultrasonic instruments, highspeed handpieces, and 3-way syringes.
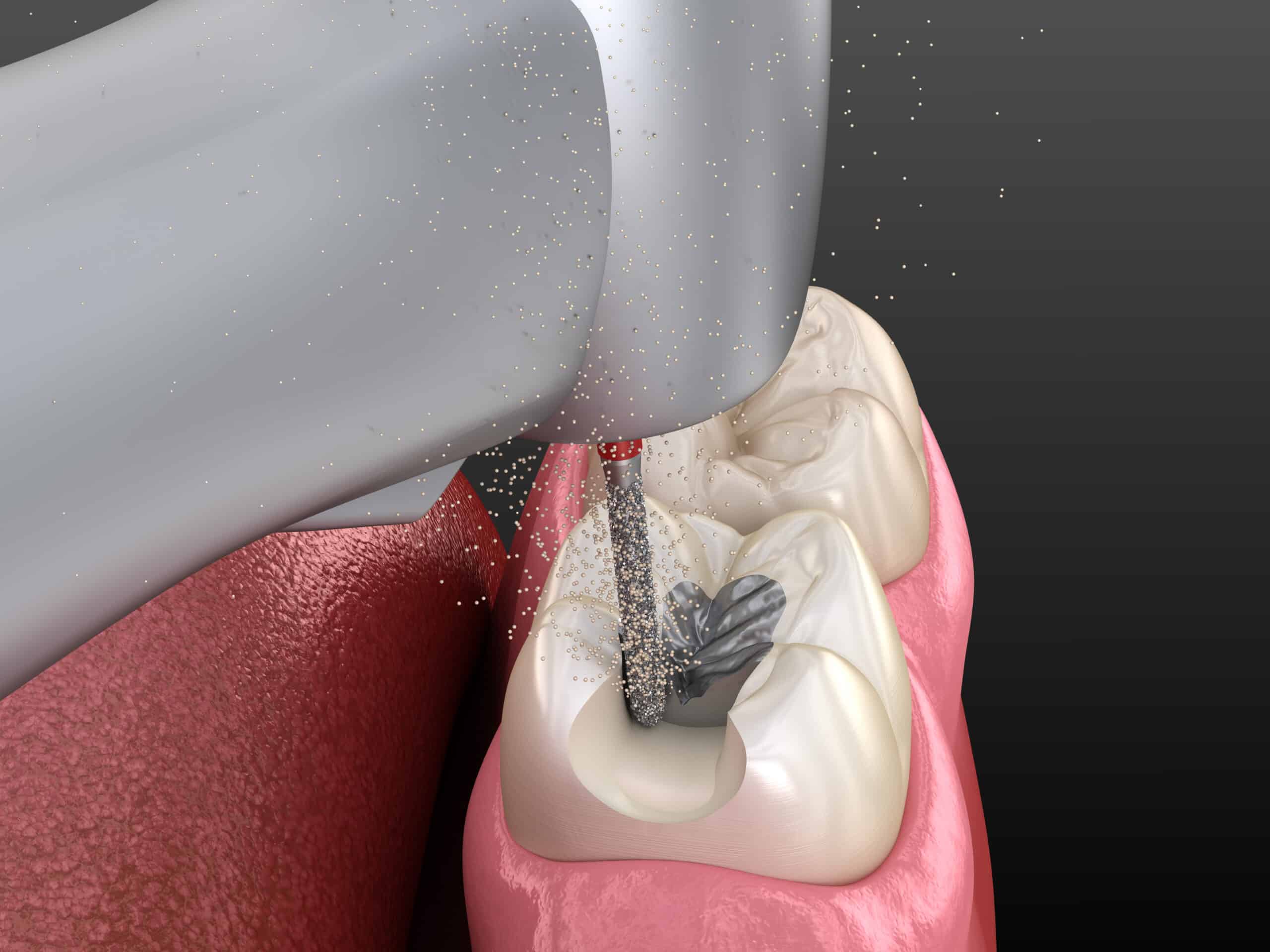
J. When performing endodontic procedure, a diluted 1% solutions of sodium hypochlorite is ideal as a disinfectant for supplies.
K. Use resorbable sutures (i.e. sutures that last 3 to 5 days in the oral cavity) to eliminate the need for a follow up appointment.
L. Disinfect surfaces with EPA-approved chemicals and maintain a dry environment.
M. Wear an N95 or equivalent or higher-level respirator such as a disposable filtering face piece respirator or a powered air-purifying or an elastomeric respirator; eye protection such as goggles, reusable face shields; gloves; and a laboratory gown.
N. The use of teledentistry in real-time video consultations is highly advised to do first. This is to determine if the patient’s oral health really needs immediate care rather than waiting for the required time period that a recovered CoVid patient is really considered safely as "recovered".
CONCLUSIONS:
We don't want CoVid-19 to rule our lives and due to our own fear deny our patients the dental treatment they need. However, we also need to take consideration of our own safety, the safety of our love ones and our staff. Thus, on this situation it is very important that we abide strictly with the proper infection control protocols and do our treatments like every patient we do is a CoVid-19 patient unless proven otherwise. Having said that, we also have to balance our decisions whether to provide non-elective dental procedures to our patients or not because as health professionals we are legally and morally bound to perform our duties to our patients and not be discriminatory. Thus, we can indeed treat a recovered CoVid-19 patient even immediately after the patient's recovery as long as we strictly follow the protocols and the process before, during and after the procedure/s to the letter, so, we can both serve and protect.
CONTRIBUTORS:
Dr. Bryan Anduiza - Writer
Dr. Mary Jean Villanueva - Writer | Editor
REFERENCES:
1. Centers for Disease Control and Prevention Guidance for Dental Settings. Interim Infection Prevention and Control Guidance for Dental Settings During the COVID-19 Response. Washington, D.C.: 2020."https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html". Accessed 7/14/2020.
2. Gugnani N, Gugnani S. Safety protocols for dental practices in the COVID-19 era. Evid Based Dent 2020;21(2):56-57.
3. Martins-Filho, Gois-Santos PRd, Tavares VT, et al. Recommendations for a safety dental care management during SARS-CoV-2 pandemic; 2020.
4. Ramoni RB, Walji MF, Kalenderian E Safety in Dentistry. Rockville, MD: AHRQ PSNet [Serial online] 2016. "https://psnet.ahrq.gov/perspective/safety-dentistry". Accessed 6/10/2020.
5. Azzi L, Carcano G, Gianfagna F, et al. Saliva is a reliable tool to detect SARS-CoV-2. J Infect 2020;81(1):e45-e50.
6. Iwasaki S, Fujisawa S, Nakakubo S, et al. Comparison of SARS-CoV-2 detection in nasopharyngeal swab and saliva. J Infect 2020.
7. Zhu J, Guo J, Xu Y, Chen X. Viral dynamics of SARS-CoV-2 in saliva from infected patients. J Infect 2020.
8. Peng X, Xu X, Li Y, et al. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci 2020;12(1):9.
9. Anderson EL, Turnham P, Griffin JR, Clarke CC. Consideration of the Aerosol Transmission for COVID-19 and Public Health. Risk Anal 2020;40(5):902-07.
10. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med 2020;382(16):1564-67.
11.Sommerstein R, Fux CA, Vuichard-Gysin D, et al. Risk of SARS-CoV-2 transmission by aerosols, the rational use of masks, and protection of healthcare workers from COVID-19. Antimicrob Resist Infect Control 2020;9(1):100.
12. Bahl P, Doolan C, de Silva C, et al. Airborne or droplet precautions for health workers treating COVID-19? J Infect Dis 2020.
13. Jayaweera M, Perera H, Gunawardana B, Manatunge J. Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ Res 2020;188:109819.
14. Centers for Disease Control and Prevention Situation Summary. Washington, D.C.: U.S. Department of Health and Human Services 2020. "https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/summary.html ". 5/21/2020.
15. Moodley R, Naidoo S, Wyk JV. The prevalence of occupational health-related problems in dentistry: A review of the literature. J Occup Health 2018;60(2):111-25.
16. Coulthard P. Dentistry and coronavirus (COVID-19) - moral decision-making. Br Dent J 2020;228(7):503-05.
17. Prevention CfDCa Frequently Asked Questions. Washington, D.C.: 2020. "https://www.cdc.gov/coronavirus/2019-ncov/faq.html#Coronavirus-Disease-2019-Basics". Accessed 6/10/2020.
18. Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N Engl J Med 2020;382(10):970-71.
19. Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020
20. Centers for Disease Control and Prevention Implementing Safety Practices for Critical Infrastructure Workers Who May Have Had Exposure to a Person with Suspected or Confirmed COVID-19. 2020. "https://www.cdc.gov/coronavirus/2019 ncov/community/critical-workers/implementing-safety-practices.html". Accessed 7/14/2020.
21. Centers for Disease Control and Prevention Discontinuation of Isolation for Persons with COVID -19 Not in Healthcare Settings. Washington, D.C.: 2020. "https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-in-home-patients.html". Accessed 6/10/2020.
22. American Dental Association ADA Interim Guidance for Management of Emergency and Urgent Dental Care. Chicago, Ill: 2020. "https://www.ada.org/~/media/CPS/Files/COVID/ADA_Int_Guidance_Mgmt_Emerg-Urg_Dental_COVID19?utm_source=adaorg&utm_medium=VanityURL&utm_content=interimguidance-flowcharts&utm_campaign=covid-19".