Are You Still Well Verse with the Various Pulpal Injury, Its Signs & Symptoms?
The Dental pulp is a connective tissue consisting of nerves, blood vessels, ground substances, interstitial fluid, odontoblasts, fibroblasts, and other cellular components. It is the part of a tooth that gives sustenance, innervation, response to temperature, dentin formation. Clinically, a normal pulp is identified as symptom-free and with normal response to pulp testing. There are cases that the pulp may not be histologically normal, yet, can be considered as “clinically” normal pulp. In fact, with a cold test, a mild or transient response can be felt lasting no more than 1 or 2 seconds after the removal of the stimulus. Moreover, we all know, it is also important that we do a comparative test between the tooth in question and its adjacent and contralateral teeth to arrive in a definitive diagnosis.
There are various modes and methods to arrive at an accurate diagnosis for pulpal disease. This diagnosis will provide us with reference to decide the best clinical approach and have a more successful prognosis.
Thus, this post will give you a guide on your diagnosis technique to properly identify the pulpal condition and, of course, our treatment options.
TYPES OF PULPAL INJURY
I. Mechanical Injury
A. Trauma
A traumatic injury refers to a physical injury with sudden onset that may or may not be accompanied by a fracture of the crown or root of the tooth.
- This type of trauma is more common in children than adults as they are generally very active.
- Direct physical force applied on the tooth such as opening bottles, pins or tearing wrapper using the teeth, nail biting and bruxism can also result in this type of trauma.
- Certain dental procedures can cause this type of trauma:
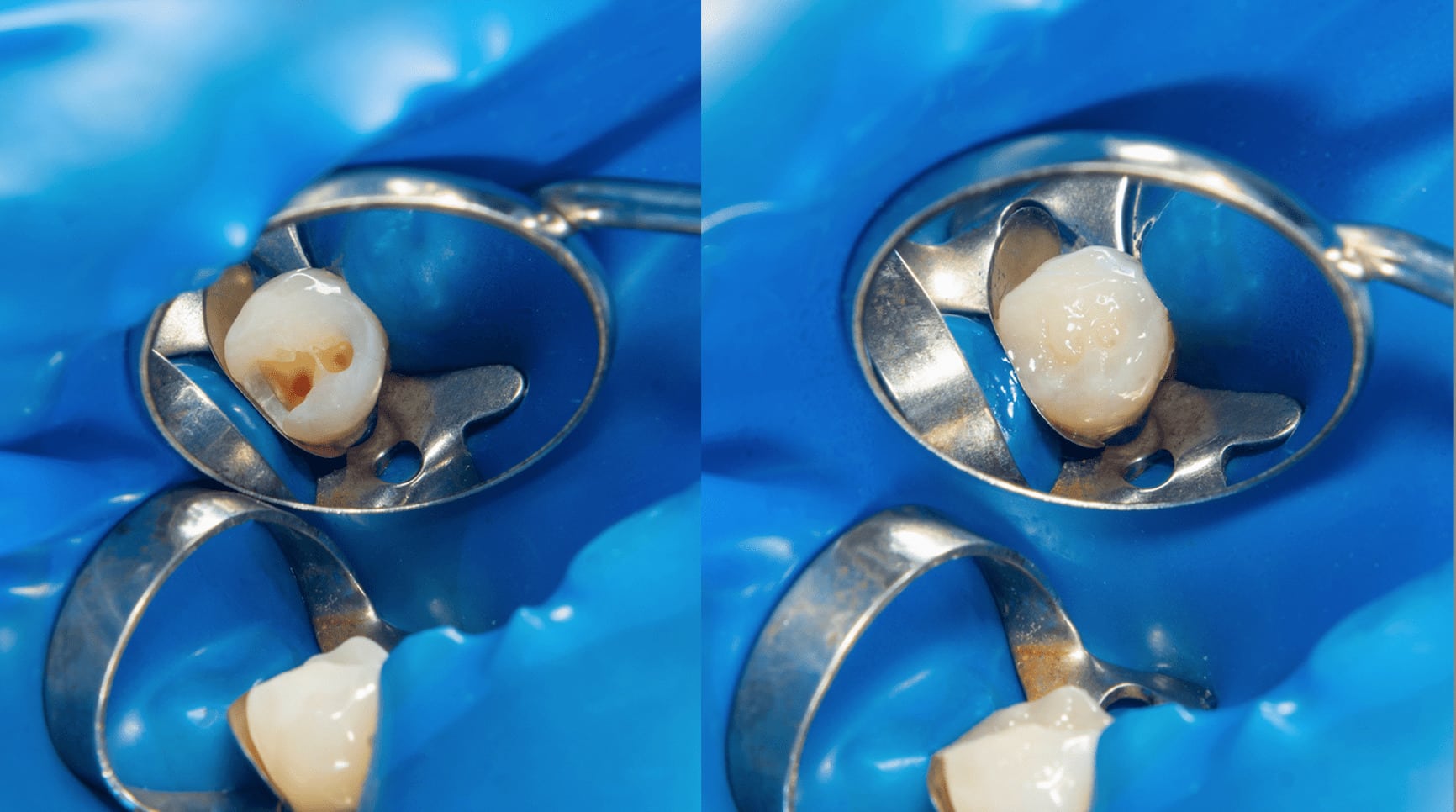
i. Exposure of the pulp during the excavation of a carious tooth structure.
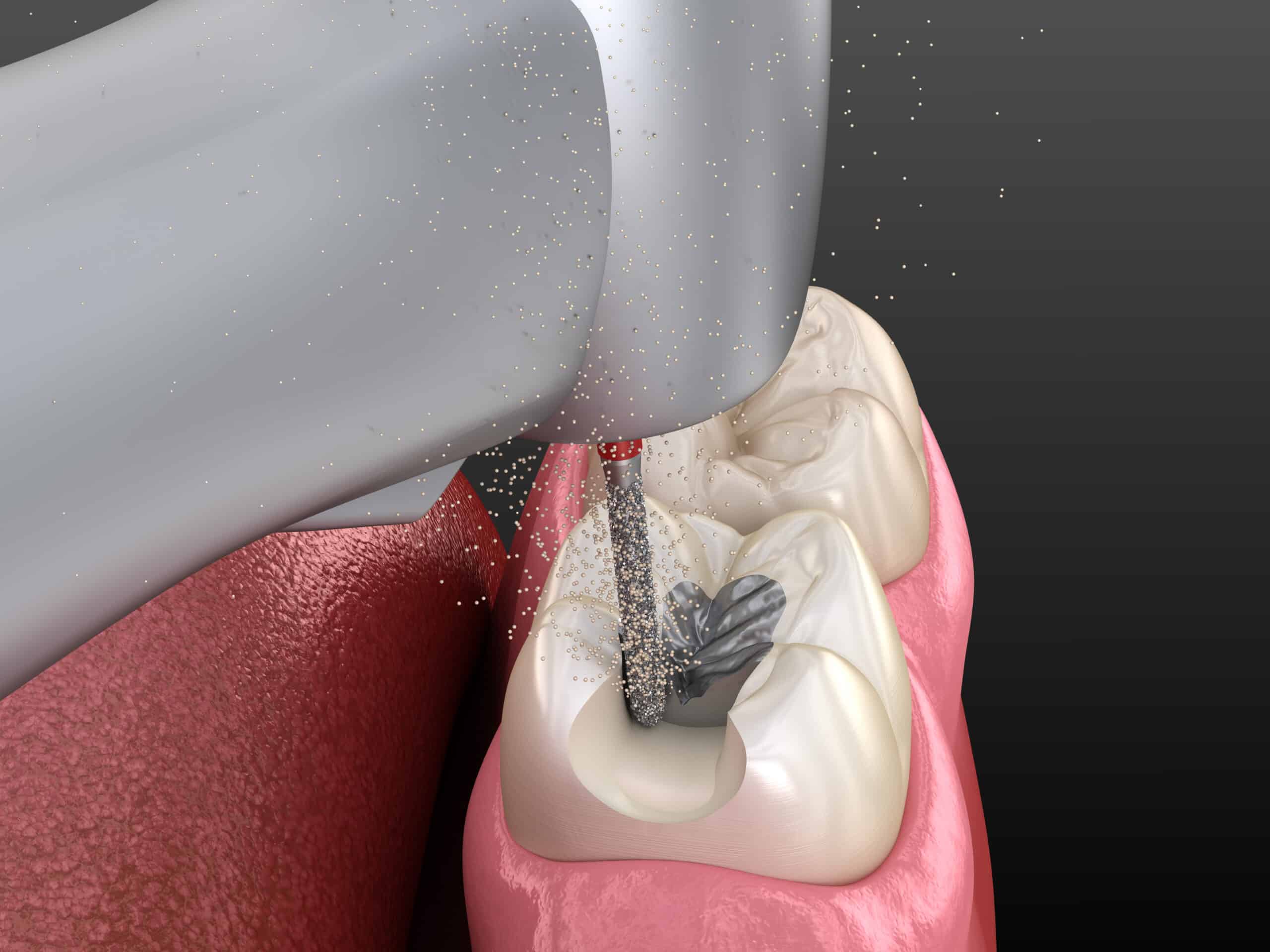
ii. The use of pins for mechanical retention of amalgam or other restoration.
iii. Rapid or strong movement of the teeth cause by orthodontic treatment.
B. Cracked Tooth Syndrome
A Cracked Tooth Syndrome is referred as an incomplete fractures through the body of the tooth that may cause pain of apparent idiopathic origin.
- The patient usually complains of pain, ranging from mild to excruciating at the release of the biting pressure.
- The most reliable diagnostic method to use is to try to reproduce the pain.
- Other diagnostic tools to identify a cracked tooth are the use of a dye or transillumination cover available to some light cure units such as VALO or use of a tooth slot during restoration.
- If the fracture is confined in the enamel and dentin only, the best restorative approach can be an inlay or onlays or crown restoration as these can immobilize or encase the tooth fracture.
C. Barodontalgia
Also known as Aerodontalgia as it denotes toothache occurring at low atmospheric pressure at high altitude.
- Tooth with chronic pulpitis can be asymptomatic at ground level, but pain can be felt at high altitude when riding an airplane. Barodontalgia has generally been observed in altitude between 5000-10000feet.
- By applying the cavity with a varnish or a base of zinc-phosphate cement, with a sub base of zinc oxide-eugenol cement in deep cavities, helps to prevent barodontalgia.
- Barodontalgia is classified by Raunch According to Chief Complaint:
Class I : Acute Pulpitis – Sharp Pain – Ascent
Class II : Chronic Pulpitis – Dull Throbbing Pain – Ascent
Class III : Necrosis – Dull Throbbing Pain – Descent, Asymptomatic – Ascent
Class IV : Periapical Abscess – Pain with Both Ascent & Descent
D. Pathologic Wear
Pathologic Wear may be identified as a tooth that becomes or nearly exposed by pathologic wear of the teeth from either abrasion or attrition if secondary dentin is not deposited rapidly enough.
II. Thermal Injury
These are injuries described as pain felt when the temperature increases. This is due to the low susceptibility of cells to heat.
- Usually this type of injuries is caused by the dentist when an error occurs in performing certain dental procedures that may lead to postoperative inflammation or necrosis of the pulp. These procedures maybe the following:
i. Heat created from cavity preparation.
ii. Frictional heat caused during polishing of a restoration.
iii. Exothermic heat from the setting of cement.
iv. Direct conduction of heat and cold through deep fillings without a protective base.
III. Chemical Injury
These are injuries caused by the use of certain pharmaceutical and non-pharmaceutical products by patients or by injudicious use of caustics by the dentist.
These are injuries caused by the use of certain pharmaceutical and non-pharmaceutical products by patients or by injudicious use of caustics by the dentist.
- These may can result to lesions on the oral cavity, yet, are rarely reported when it happens. Thus, it becomes important that we understood the information about the product we use in our treatments and we provide necessary instructions to our patients for prevention of this to occur, if needed.
- These burns may be self-inflicted, induced by allergic reaction or can be iatrogenic.
- Detailed history is the key to diagnosing and managing this type of injury.
- Chemical injuries are usually treated by eliminating the causative factor and dentist can manage it, if it occurs, through palliative therapy.
- Arsenic in silicate restorations and desensitization paste are the most frequent cause of pulp death.
- Key factors that would determine pulpal reaction to restorative materials are the following:
i. Acidity (pH of the material).
ii. Absorption of water during setting reaction.
iii. Poor marginal adaptation of material.
IV. Bacterial-Caused Injury
It is suggested that bacteria can be a possible cause of pulp inflammation. The presence or absence of bacterial irritation will determine the pulp survival.
- Most of the bacteria recovered from infected vital pulps are streptococci and staphylococci.
- Other micro-organisms, including anaerobes can be present in isolated areas.
- Lactobacilli are commonly found in carious dentin.
- Broad spectrum antibiotic and the use of Chlorhexidine can be used to further eliminate or control the harmful bacteria inside the oral cavity.
CONCLUSION
On the initial injuries to the pulp mentioned on this post, it is very clear that we, as dentists, can also be a causative factor. Thus, it is imperative for us to really read and understand the instruction of the equipment and chemical treatments, we may use to perform our dental procedure. Please read our Part 2 next week as we delve more into this subject as well as recommended treatments for these type of pulpal injuries.
CONTRIBUTORS
Dr. Bryan Anduiza - Main Writer
Dr. M. Jean Villanueva - Writer | Editor