HOW APPLICABLE IS COLD STERILIZATION IN THE CURRENT INFECTION CONTROL?
Its has been taught in school that the use of high level of concentration disinfectants or sterilants can be a part of instrument reprocessing protocol. And, Glutaraldehyde has been the "go-to sterilant" for years. It is classified as a high-level disinfectant. Its properties as a chemical sterilant were initially recognized in the early 1960s as an effective bactericidal solution. On this article, we will delve into relevant information, so, we to decide for ourselves based on evidence if these solutions like Glutaraldehydes or even this method, for that matter, is still even relevant to be part of our infection control procedure.
INFORMATION
The term "cold sterile" comes primarily to instruments that can be disinfected and can be considered "sterile" if the instruments or items are left in the solution for a certain prescribed time specified by the manufacturer. According to CDC, a minimum of 10 hours at least that the instruments should be immersed to the solution at 20–25°C in order to be considered as sterile in case of Glutaraldehyde solution. Generally, cold sterilization is an alternative method to use for types of instruments that are considered heat sensitive and would be damaged by placing them in a steam autoclave, unsaturated chemical vapor sterilizer, or in a dry-heat sterilizer.
HANDLING
When using this type of chemical disinfectants or sterilants, proper PPEs must be observed for the protection of the one doing the process. This means wearing of gloves, mask, safety eye wear, and isolation gown or lab coat or apron during handling is a MUST NOT AN OPTION. The room or area of sterilization must have proper ventilation and whatever chemicals or equipment we use to do our infection control, one must always follow the manufacturer’s instructions. Standard precautions is necessary as we need to treat these chemicals with caution not only because of its health risks that's been recorded through the years but, especially in the current situation wherein there's still a lot of unknown about CoVid-19. In our sterilization area, we must think that everything in that room is harmful to ensure your safety and your staff's.
CLASSIFICATION
According to the Center for Disease Control and Prevention (CDC), dental instruments are classified into three categories according to the risk of transmitting infection. This classification is something you can use in identifying which instrument works with what type of reprocessing procedure and which doesn't. The classification is categorized into critical, semi-critical, and noncritical and are based on the following criteria:
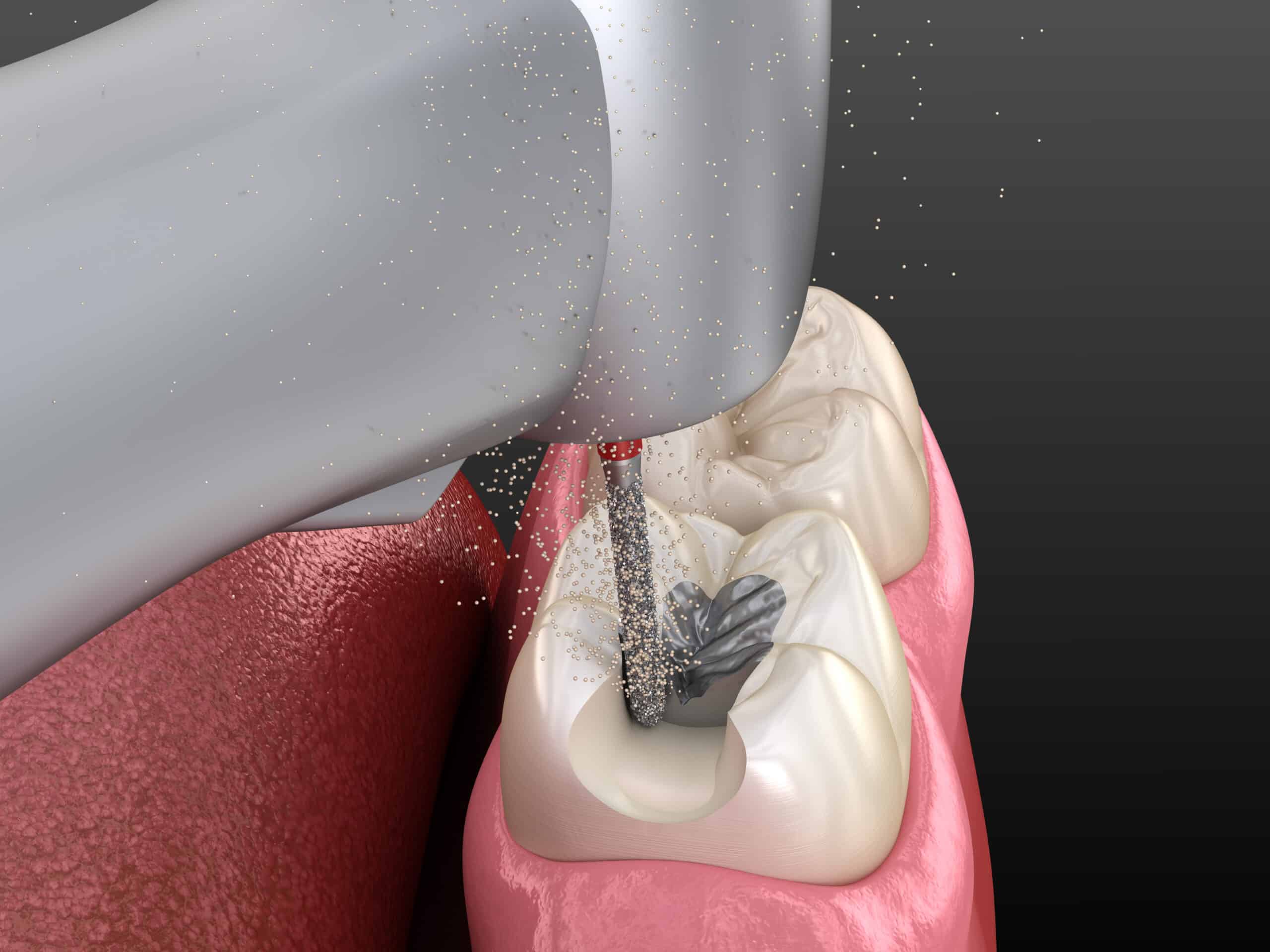
A. Critical Instruments
These are instruments that are used to penetrate soft tissue or bone, or enter into or contact the bloodstream or other normally sterile tissue. They should be sterilized after each use. Sterilization is achieved by steam under pressure (autoclave), dry heat, or heat or chemical vapor. Critical instruments include forceps, scalpels, bone chisels, scalers, highspeed handpieces and burs.
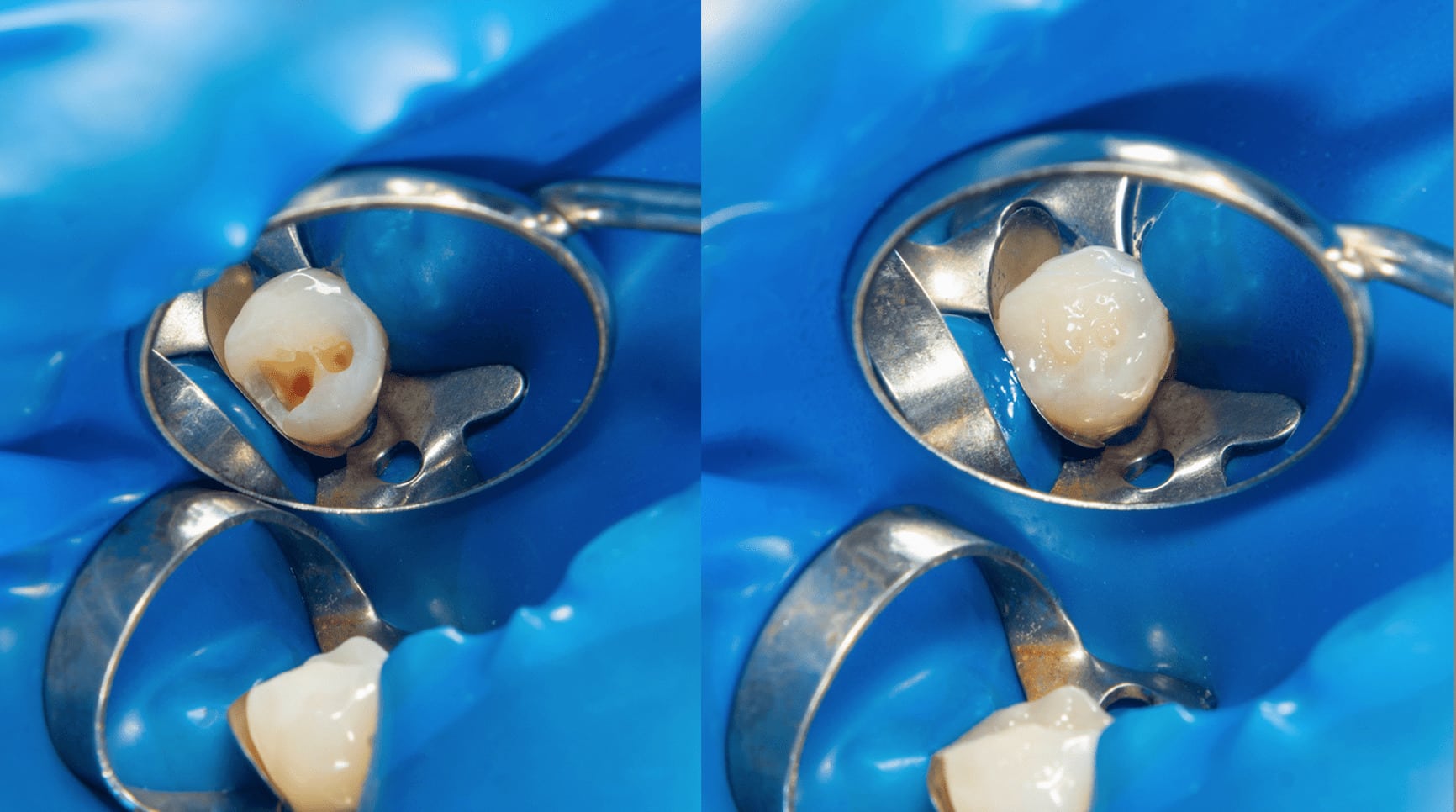
B. Semi-Critical Instruments
These are instruments that do not penetrate soft tissues or bone but contact mucous membranes or non-intact skin. These include mirrors, reusable impression trays, and amalgam condensers. These devices should also be sterilized after each use. In some cases, however, sterilization is not feasible and, therefore, high-level disinfection is appropriate. A chemical solution can only be considered a high level disinfectant or sterilant when it has a label from EPA (Environmental Protection Agency) as indeed a “sterilant/disinfectant”.
C. Non-Critical Instruments
These are those that come into contact only with intact skin. These include the external components of x-ray heads, blood pressure cuffs, and pulse oximeters. Such devices have a relatively low risk of transmitting infection. Therefore, they may be reprocessed between patients by intermediate-level or low-level disinfection. An intermediate-level disinfectant is EPA-registered as a “hospital disinfectant” and will be labeled for “tuberculocidal” activity (e.g., phenolics, iodophors, and chlorine-containing compounds). A low-level disinfectant is EPA-registered as a “hospital disinfectant” but is not labeled for “tuberculocidal” activity (e.g., quaternary ammonium compounds).
DISADVANTAGES
Cost is part of our consideration when we practice our profession. This affects many things when we make decisions and, of course, very much related on how we charge our patients. One of the advantages of cold sterilization is its low cost. Some may not be cheap but it certainly beats the price doing other methods of sterilization. However, what we forget sometimes that though it can be relatively cheap, using them for sterilization can also result to damage of some of our instruments if exposed to these solutions for a longer period of time like our dental instruments such as burs that maybe made of alloy rather than stainless steel. We may have saved a few cents doing this type of sterilization but if we will follow the correct time of immersion for this to act as a sterilizer, we can also lose money at the end of the day on the cost of certain dental instruments that can be damaged by it.
The biggest disadvantage of these “chemical immersion sterilants” such as Glutaraldehydes is that it can be toxic and allergenic to those healthcare workers who use them. In the years since its introduction as a disinfectant/sterilant, Glutaraldehyde has been linked with a variety of adverse health effects including asthma, nausea, respiratory irritation, and skin rashes. There are even cases wherein long-term exposure to these chemicals result to untoward health conditions that can be permanent to our over-all health.
CONCLUSION
As dental professionals especially nowadays, it is indeed difficult to stay afloat with all the costs to protect ourselves, our staff and our patients. Thus, cold sterilization can be an inviting or tempting alternative for our method of sterilization. However, it is very important to take note that even before CoVid-19, a chemical solution in order to be considered as an effective sterilization medium, the instruments must be exposed to the solution for a long time at an average of at least 3-6 hours or even more depending on the manufacturer's recommendation. Initially, we use them as many of our instruments are heat sensitive, but, this has changed enormously through the years. Our point is that, although, we do understand that there are times when we prioritize cost more than anything else when we make business decisions in our dental practice, but, there should also be a time when safety must trump financial gain at all cost.
CONTRIBUTOR:
Dr. Bryan Anduiza - Researcher | Writer
Dr. Mary Jean Villanueva - Writer | Editor