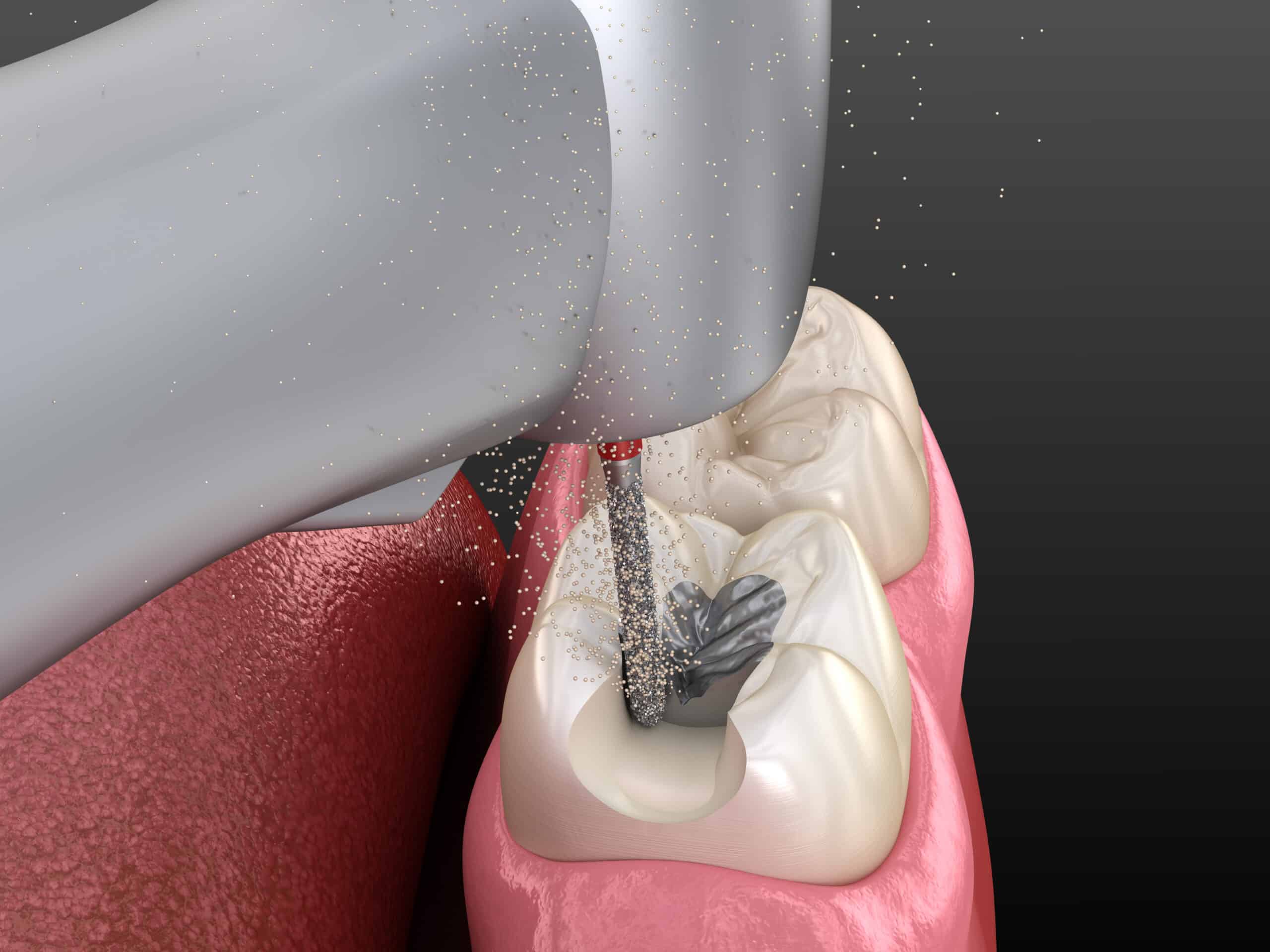
WHAT IS THE IMPORTANCE OF KNOWING AND UNDERSTANDING ANTICOAGULANTS IN OUR DENTAL PRACTICE?
As DMD Center team discussed what topic we should do on our post for this week, the issue of anticoagulants arose and became interesting for us to tackle because we felt that sometimes, we, as dentists forget to ask the current medicines that our patients regularly take or even temporarily is taking to address certain medical conditions. There are also instances that we see a history of a health condition but we are not familiar with the drugs or its effect to the body, thus, we end up ignoring this nugget of information and make mistakes in not addressing this detail especially if we felt that our procedure is just very simple like oral prophylaxis, but, in reality may hinder the success of our treatment. . On this 3 part posts, we will delve deeper on the issue of blood clotting and anticoagulant meds that our patients maybe taking that can result from mild to severe side effect/s.
In reality, we and/or our patients sometimes forget to really take time and stock the details that medical and dental history provide us prior to discussing to our patients the treatment we will implement on them. So, it is only when an unexpected or untoward side effect/s happens that we do check again the medical and/or dental history of our patient. If we will be quite honest, this is actually one of the good things that CoVid-19 pandemic brought in our dental practice. We became more conscious, conscientious and careful in our history taking. As the saying goes, “the devil is on the details”.
KNOWING ANTICOAGULANTS
Anticoagulants drugs are agents that reduce the ability of the blood to coagulate or form clots. They also interfere with chemicals needed to make clots or clotting factors. Thus, it is important to initially know the effects of these drugs to our body.
Let’s take these medicines as examples: Warfarin, Acenocoumarol and Phenindione block the effects of vitamin K, which is needed to make some clotting factors described earlier. Blocking vitamin K prevents blood clots forming so easily by increasing the time it takes to make fibrin. It usually takes two or three days for these medicines to work fully.
While Dabigatran, Apixaban, Edoxaban and Rivaroxaban prevent a blood chemical called thrombin from working, which in turn prevents fibrin from being made from fibrinogen. Dabigatran binds to thrombin. Apixaban and rivaroxaban stop thrombin from being made. All four medicines work quickly - within two to four hours.
THE BLOOD CLOTTING PROCESS
Blood clotting is a natural process triggered in response to damaged blood vessels from injury, trauma or invasive procedures. When an injury occurs, platelets are activated, resulting in an increased tendency to adhere to each other and to the damaged blood vessel which creates primary hemostasis. During this process, a series of reactions occurs initiating the conversion of inactive coagulation factors to their active forms, ultimately leading to produce fibrinogen. Now fibrin stabilizes and gathers all the platelets to the damage blood vessel wall to prevent further blood loss.
I. Normal Control of Bleeding
The three phases of haemostasis for controlling bleeding are vascular, platelet and coagulation phases. The coagulation phase is followed by fibrinolytic phase that dissolves the clot.
A. Vascular Phase (In Seconds)
Any injury triggers vascular phase, which consists of:
- Vasoconstriction of arteries and veins in the area of injury.
- Retraction of cut arteries.
- Build-up of extra vascular pressure by blood lost from cut vessels.
B. Platelet Phase (Primary Hemostasis-In Seconds)
- Platelets and vessel walls become sticky.
- Mechanical plugs of platelets seal off openings of cut vessels.
C. Coagulation Phase (Secondary Hemostasis-In Minutes)
- Blood lost into surrounding areas coagulates through extrinsic and common pathways.
- Blood in vessels in areas of injury coagulates through intrinsic and common pathways.
- Takes place more slowly than other phases.
D. Fibrinolytic/Metabolic Phase
- It is activated simultaneously with the coagulation and functions to maintain fluidity of blood during coagulation.
- It also serves in clot lysis once tissue repair begins.
- Anti-thrombotic agents are released.
- Spleen and liver destroy these anti-thrombotic agents.
The coagulation cascade involves the intrinsic, extrinsic, and common pathways, which have been found to be highly interconnected. The intrinsic pathway requires the clotting factors VII, IX, X, XI, and XII. The extrinsic pathway is initiated with the release of tissue factor II. The common point in both pathways is the activation of factor X to factor Xa. Factor Xa activates prothrombin (factor II) to thrombin (factor IIa). Thrombin, in turn, converts fibrinogen to fibrin.
IDENTIFY PATIENTS AT RISK OF BLEEDING
I. Presence of Medical History Of:
- Bleeding problems in relatives.
- Bleeding problems after surgery, tooth extraction and trauma.
- Medications: Aspirin, anticoagulants, long term antibiotics.
- Illnesses associated with bleeding problems: Leukemia, congenital heart disease, liver disease, hemophilia
- Spontaneous bleeding
II. With Clinical Findings Of:
- Jaundice, Pallor
- Spider Angiomas
- Ecchymoses, Petechiae
- Oral Ulcers
- Hyperplastic Gingival Tissue
- Hemarthrosis
III. Base on Screening Laboratory Test Results:
- Platelet Count
- Ivy Bleeding Time (BT)/PFA
- Prothrombin Time (PT)&INR
- Activated Partial Thromboplastin Time (aPTT)
- Thrombin time (TT)
LABORATORY EXAMINATION FOR BLOOD CLOTTING ASSESSMENT
I. Quantitative (Platelet Count):
- Normal Platelet Count-150,000~440,000/mm 3
- Thrombocytopenia-Platelet <150,000/mm 3
- Severe IntraOp Bleeding-Platelet <40,000~70,000/ mm 3
- Spontaneous Bleeding-Platelet <20,000/mm 3
- Minimal Recommended PreOp Platelet >75,000/mm 3
However, qualitative difference makes it unwise to rely solely on platelet count
II. Qualitative (Platelet Function):
- Ivy Bleeding Time-Normally 1~6 mins
- Closure Time from PFA 100-Normally 60~120 seconds
Ivy Bleeding Time
In the Ivy method, a blood pressure cuff is placed on the upper arm and inflated to 30 mm of Hg. A lancet or scalpel blade is used to make a stab wound on the underside of the forearm. An automatic, spring-loaded blade device is most commonly used to make a standard-sized cut. The area stabbed is selected so that no superficial or visible veins are cut. As these veins, because of their size, may have longer bleeding times, especially in people with bleeding defects. The time from when the stab wound is made until all bleeding has stopped is measured and is called the bleeding time. Every 30 seconds, filter paper or a paper towel is used to draw off the blood. The test is finished when bleeding has stopped completely.
Dentists should be able to order and interpret appropriate laboratory tests when minor oral surgery is required for patients taking anticoagulants or problems with blood clotting. So, what are the laboratory tests commonly used for those with coagulation disorders? Prothrombin Time (PT) and International Normalized Ratio (INR).
I. PT-Activated by Tissue Thromboplastin.
The PT measures the effectiveness of the extrinsic and common pathways. The normal value is approximately 10 to 15 seconds. Because of the variability in PT reported by different laboratories, it is no longer considered adequate to use PT to monitor the level of anticoagulation. In order to reduce variability, INR was developed as a consistent test for measuring anticoagulation status. INR is the more reliable and consistent measure. A normal individual should have an INR of 1.0
II. International Normalized Ratio (INR)
Dependent upon the medical condition, physicians will prescribe anticoagulant medication so that patients demonstrate an INR in a therapeutic range of approximately 2.0 to 3.5. These conditions include states in which thromboembolism could cause serious morbidity or death, such as post myocardial infarction, and prevention of deep venous thrombosis (DVT). Additionally, patients with atrial fibrillation are anticoagulated because of the greater likelihood of blood clot formation due to turbulent blood flow through the heart. In those individuals with prosthetic heart valves and certain hypercoagulable states, the INR should be approximately 3.5. If the dentist encounters a patient with an INR greater than 4.0, the patient should be referred to the physician for evaluation. An INR greater than 4.0 is usually considered nontherapeutic, and the patient is at risk for serious bleeding complications.
Equation for Calculation of INR:
INR = (patient PT/mean normal PT) ISI
ISI = International Sensitivity Index, assigned to the test system
Normal Values:
PT = 11-15 secs, INR = 1.0-1.2
There is a current Portable Systems for Rapid Measurement of PT and INR
Portable systems for rapid measurement of PT and INR have been specifically designed for healthcare professionals and their patients to enable on-the-spot analysis of coagulation levels (PT/INR) during mobile emergency treatment or for routine follow-up in a hospital ward and/or at their general practice. These systems are easy-to-use reflectance photometers, portable and battery-powered devices for rapid measurement of Prothrombin Time (PT) and International Normalized Ratio (INR). It has always been a challenge to health care professionals and to their patients which involves a venous blood sample or the patient themselves being sent to a laboratory. This is time-consuming and patient's compliance can be limited, as it often requires a second appointment with the healthcare professional. These systems provide accurate results from a single drop of capillary blood from the fingertip within one minute improving compliance.
There are also other laboratory examinations that maybe used to identify patients with coagulations disorders:
III. Activated Partial Thromboplastintime (aPTT)
Initiated by phospholipid platelet substitute and activated by addition of contact activator (kaolin)
Tests intrinsic and common pathways
Normal value: 25-35 secs
Thrombin time (TT):
Tests the common pathway, thus the ability to form initial clot from fibrinogen.
Normal Value: 9-13 secs
It is important to take note that control should be run for all the above mentioned tests base on the following:
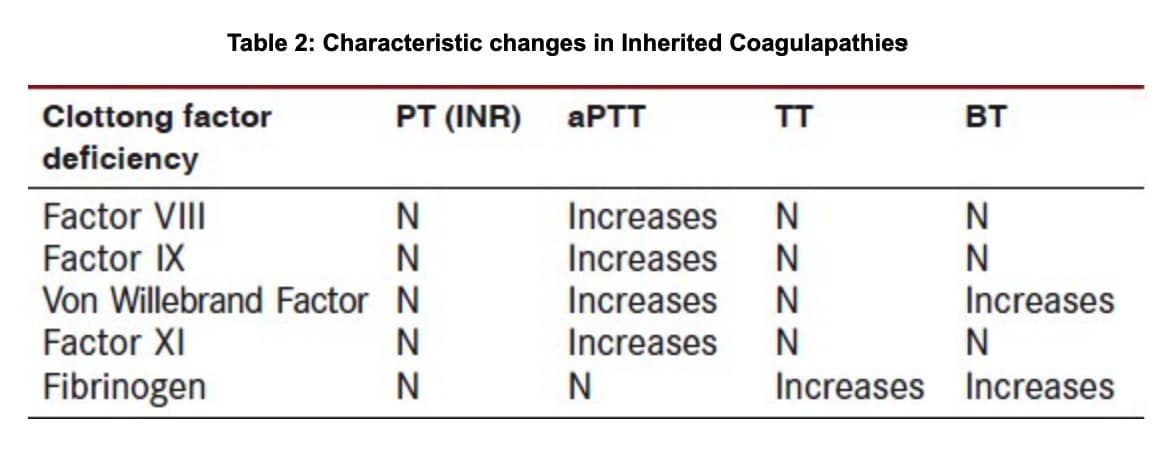
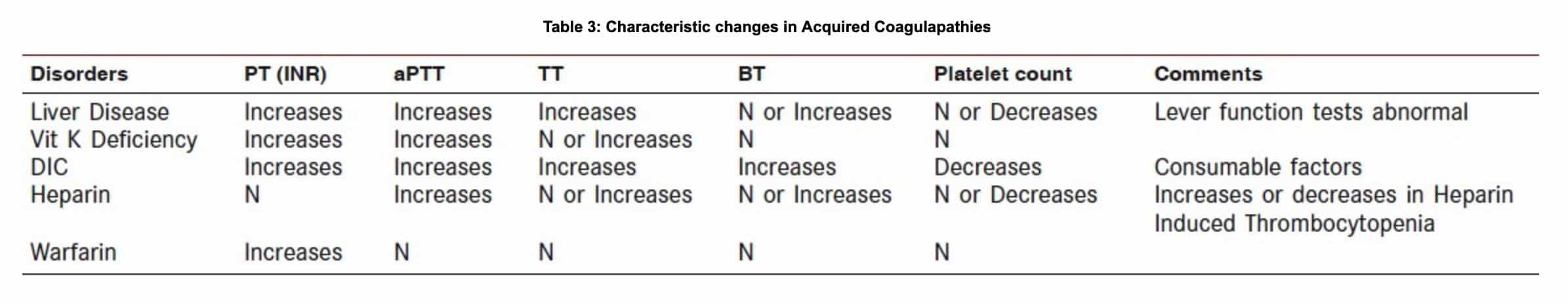
- Characteristic Changes in Inherited Coagulapathies:
Table is courtesy of Journal of ICDRO
IV. Thromboelastography (TEG)
Thromboelastograph is an instrument that measures the development of blood clot viscoelastic strength over time. A rotating piston is suspended in a cuvette filled with heated blood. As clot formation proceeds, the rotation of the piston is affected and characteristic curves are generated by the Thromboelastogram instrument used and its tracing. TEG assesses the whole blood clotting system.
Thromboelastogram- Normal Parameters
- R: Period of time from the initiation of the test to initial fibrin formation
- K: Time from the beginning of clot formation until the amplitude of TEG reaches 20 mm, representing the dynamics of clot formation.
- α angle: Angle between the line in the middle of the TEG tracing and the line tangential to the developing body of the tracing, representing the kinetics of fibrin cross linking.
- MA (Maximum Amplitude):Reflexes the strength of the clot, which is dependent on the No. and function of platelets and their interaction with fibrin.
- A60:Measures the rate of amplitude reduction 60 min after MA, representing the stability of the clot.
MEDICAL CONDITIONS THAT REQUIRES ANTICOAGULANT MEDICATIONS
There are a number of medical conditions requiring the use of anticoagulants. Some of the most common cases include cardiovascular diseases (e.g. cardiac arrhythmia, recent heart attack, etc), cerebrovascular disease (recent stroke), deep vein thrombosis and other patients with hypercoagulable state. These patients may be at risk for uncontrolled perioperative bleeding risk.
In such cases, it is imperative to know the complete and recent medical history, details of prescribed and non-prescribed medications that they are taking before the start of any procedure. For patients undergoing an invasive procedure, it is advised to secure a medical clearance first from their physician. Through this clearance, there is a clear communication between doctors on how to manage the patient efficiently during the course of the treatment.
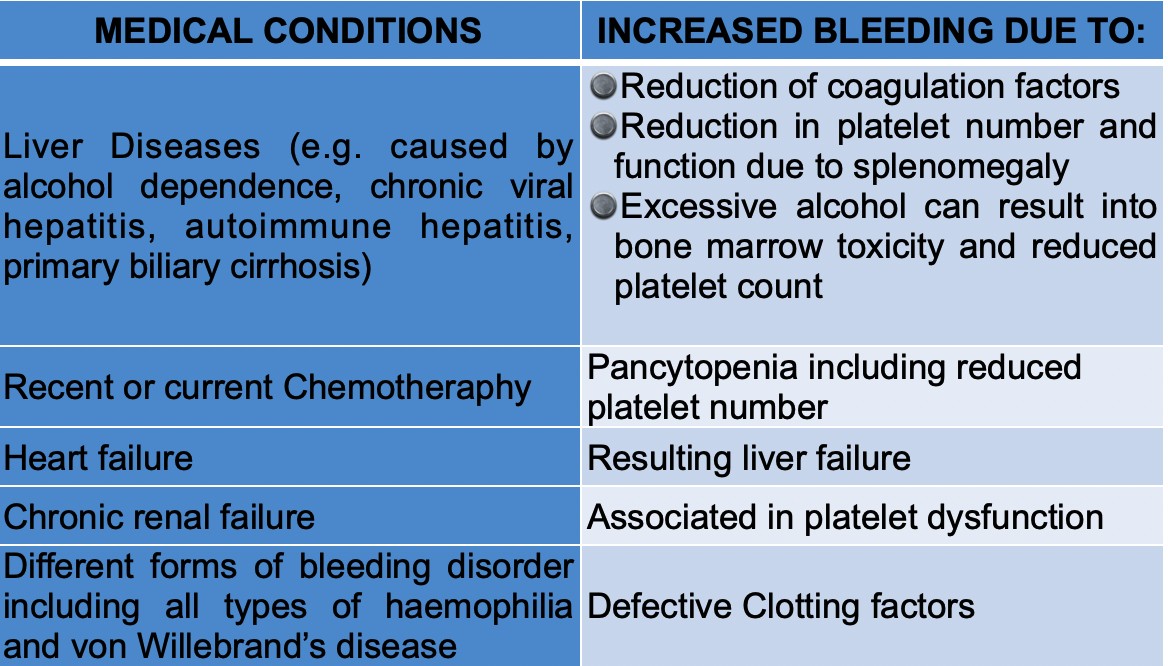
Other medical conditions not requiring anticoagulants but may increase the risk of bleeding.
CONCLUSION
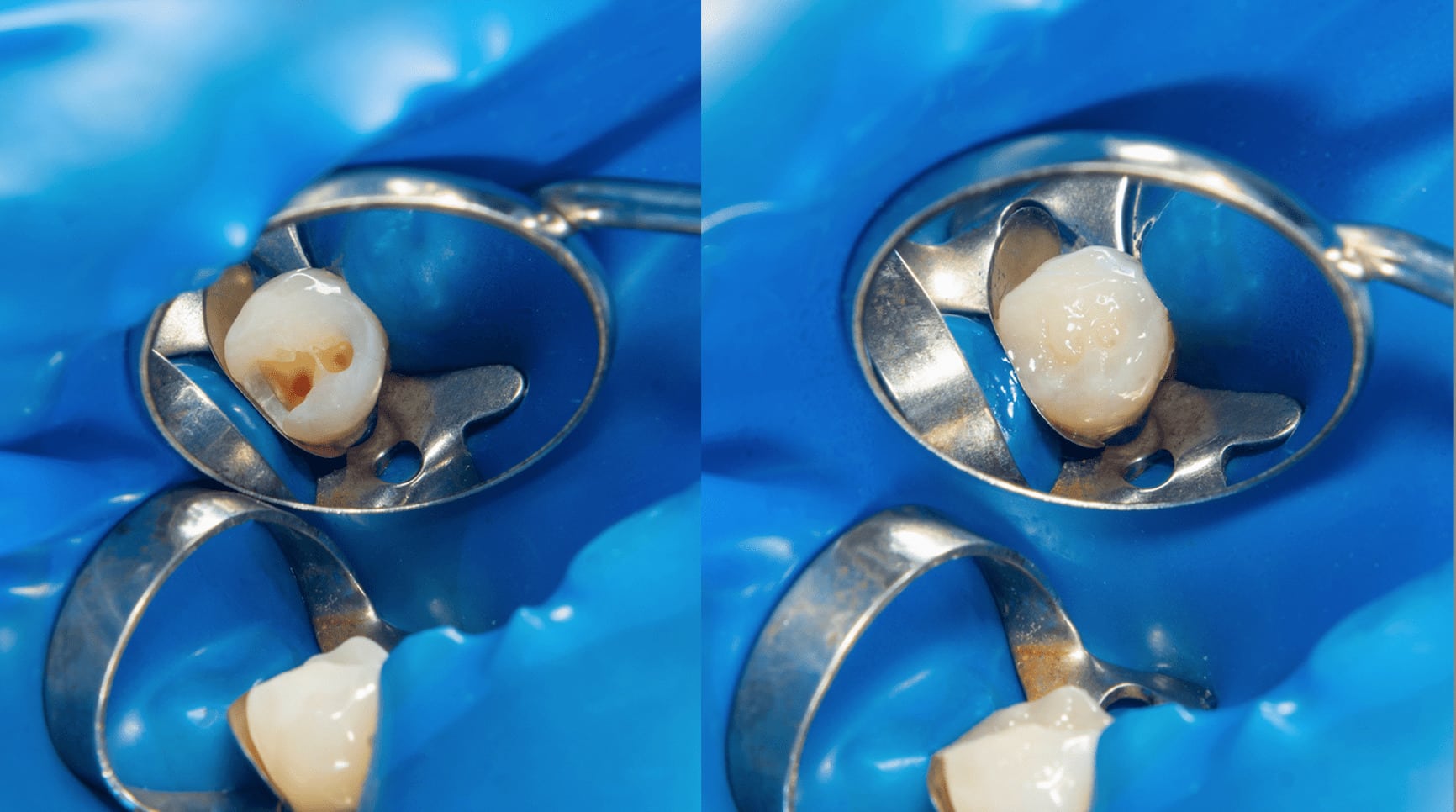
It is very significant that as dentist that do dental procedures that may result to untoward result in terms of the overall health safety of our patients know about these things. These are information that we may delegate as non-essentials especially if we deemed that the procedure we will do to our patient may have no or little bearing with this situation, contrary to reality. Thus, it is important to take note that patients with blood disorders or taking anticoagulant meds may not experience a normal healing process even with dental procedures that we do deem basic and non-surgical. So, if we want to be thorough knowing more about this will enhance your patient care especially in prescribing meds and consideration on dental treatments that may require medical clearance from their doctor prior to any of our dental treatment. At the end of the day, it is always prudent to be safe than sorry as we put the well-being of our patients into our hands.
Contributor:
Dr. Bryan Anduiza – Writer
Dr. Jean Galindez – Writer | Editor
REFERENCES:
1. Little JW, Falace DA, Miller CS, Rhodus NL, editors. Dental Management of the Medically Compromised Patient. 8 th ed.; 2012.
2. Morgan GE Jr, Mikhail MS, Murray MJ, editors: Clinical Anaesthesiology. 5 th ed. Lange; 2013.
3. Allman KG, Wilson IH, editors. Oxford Handbook of Anaesthesia. 3 rd ed. Oxford: Oxford University Press; 2010.
4. Gupta A, Epstein JB, Cabay RJ. Bleeding disorders of importance in dental care and related patient management. J Can Dent Assoc 2007;73:77-83.
5. In: Duke J, editor. Anesthesia Secrets. 4 th ed. Elsevier; 2010.
[dvk_social_sharing] [et_bloom_inline optin_id="optin_1"]