BACK TO BASICS ON NERVE BLOCKING TECHNIQUES
In our dental practice, the use of local anesthetics is an effective pain management. Most of the our dental procedures requires the use of it. As such, it became the backbone of pain control in our dental profession. Thus, it is necessary that we administer these in the safest way possible. We can achieve this by choosing the best technique related to the case at hand. And, how to administer it . Unfortunately, on certain cases, some dentists face certain challenges. Some have difficulty in identifying the anatomical landmarks especially in nerve block technique. This may lead to failure or even worse, error that can lead to severe complications. Thus, we will tackle on this post the different nerve blocking techniques and their anatomical landmark and administration guide.
A nerve block is an injection which anaesthetises the nerve trunk as it runs in soft tissue, either before it enters the jaw bone or after it leaves it to reach the teeth and associated parts. Pain sensations from every part supplied by the nerve are blocked at the site of injection and cannot reach the brain. A nerve block is used when it is necessary to anaesthetise several teeth in one quadrant or where a local infiltration cannot work.
MIDDLE SUPERIOR ALVEOLAR NERVE BLOCK
The recommended needle to use is 25-27 short gauge that penetrates about 5 mm with its tip approximately above the apex of the maxillary second premolar. After careful aspiration, half of the full cartridge should be slowly administered. The MSA nerve is often absent in many patients and if this is the case, Anterior Superior Alveolar (ASA) injection is the better choice to anaesthetise the premolar region. The Middle Superior Alveolar (MSA) injection anaesthetises the following areas:
- Mesiobuccal Aspect of the Maxillary First Molar
- Both Premolars
- PDL
- Buccal Bone
- Periosteum, along with the Soft Tissue Lateral to this Area
POSTERIOR SUPERIOR ALVEOLAR NERVE BLOCK
The recommended needle to use is 16-20 short gauge, although, 25-27 gauge is acceptable. The area of insertion is the height of the mucobuccal fold above and distal to distobuccal root of the last molar present in the arch. Needle is inserted distally and superiorly at approximately 45 degrees to the mesiodistal and buccolingual planes. The depth of insertion is approximately 15 mm following careful aspiration with 1.0 ml of solution slowly deposited to the area.
The common complications of PSA is hematoma as its landmark is close to the Maxillary artery. Pushing the needle too far may hit the pterygoid plexus or maxillary artery.
The Posterior Superior Alveolar (PSA) injection anaesthetises the following areas:
- Maxillary Molars Except for the Mesiobuccal aspect of the First Molar
- Periodontal Ligament (PDL)
- Bone
- Periosteum
- Buccal Soft Tissue Adjacent to These Teeth
ANTERIOR SUPERIOR ALVEOLAR NERVE BLOCK
Also known as the Infraorbital Nerve Block. A slow deposition of 1.0 ml of solution after aspiration into the infraorbital canal through the infraorbital foramen. The depth of penetration is similar to that of the MSA injection, however, the penetration is over the maxillary canine.
This nerve block is just an option to use if MSA is not feasible to do because it may cause psychological fear and anxiety due to the location of insertion. Moreover, the tissues on this area are very tender as they are close to the nasal region (nose), thus, may create more discomfort on the patient.
Do take note that crossover innervation should be considered in case there’s inadequate anesthesia near the midline.
The Anterior Superior Alveolar (ASA) injection anaesthetises the following areas:
- PDL
- Alveolus
- Periosteum
- Buccal Gingiva
- Maxillary Anterior Teeth
GREATER PALATINE NERVE BLOCK
The entrance to the greater palatine foramen may be palpated as a depression or soft spot in the posterior area of the hard palate. It is usually located halfway between the gingival margin and the midline of the palate, approximately opposite the distal of the maxillary second molar. The needle will penetrate through the epithelium, and the needle will appear to “fall into” a space of less resistance. The needle should be inserted until bone is contacted. Topical anesthetic must be applied for at least 1 minute while pressuring the topical solution in the sight of injection. The depth of penetration is usually less than 2-5 mm. After aspiration, 0.5 mL of anesthetic solution is very slowly deposited and observe blanching on the area to see if it worked.
The Greater Palatine Nerve Block injection anaesthetises the following areas:
- Tissues of the Hard Palate from its Most Distal Aspect and Lateral to the Midline
<p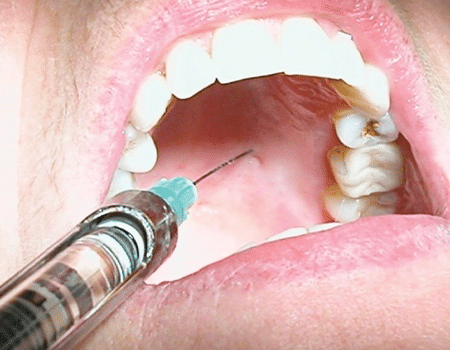 </p
</p
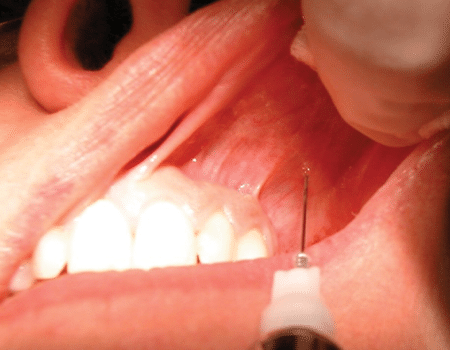
NASOPALATINE NERVE BLOCK
It is recommended to use a needle with 25-27 short gauge. The entrance to the nasopalatine foramen is at the incisive papilla, which may be visualized posterior to the maxillary central incisors. The first step is to deposit 0.3 ml of local anesthetic in the maxillary anterior midline. Then, with the needle at a 45-degree angle to the soft tissue, slowly penetrates it as the anesthetic solution is integrated to the site ahead of the needle. Once the nasopalatine area is blanched, the final needle puncture is given. The needle tip should contact the soft tissue at the lateral aspect of the incisive papilla with a depth of penetration of 1-2mm at the bony endpoint. Approximately 0.25 ml may be very slowly introduced after aspiration.
The Nasopalatine Nerve Block injection anaesthetises the following areas:
- Tissues of the Palatal Aspect of the Premaxilla
- Maxillary Incisors
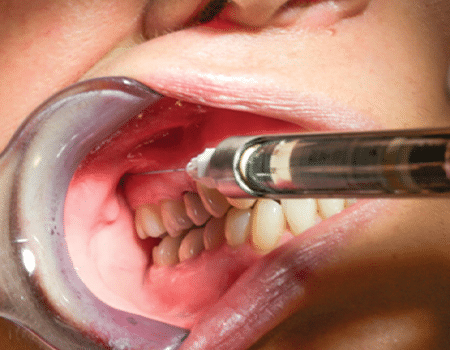
INFERIOR ALVEOLAR NERVE BLOCK
The Inferior Alveolar (IA) injection is also referred to as Mandibular Nerve Block. In an IA block, a long needle is positioned parallel to the mandibular occlusal plane and from the contralateral premolar area between two premolars to a point on the soft tissue approximately 1.5 cm above the mandibular occlusal plane. The IA Nerve Block is described with an insertion point 1.0 cm above the mandibular occlusal plane. The mucosa is pierced at a point between the pterygomandibular raphe and the deep tendon of the temporalis muscle, and the needle is advanced until bone is contacted, usually about 25 mm.The best way to visualize the lateral positioning of the needle prior to penetrating soft tissue is to look for the depression seen on the immediate lateral aspect of the pterygomandibular raphe, the coronoid notch ( the greatest concavity on the anterior border of the ramus) forming a small triangle. Once the needle is advanced and bone contacted, the tip should now be just superior to the lingula. The needle should be withdrawn 1–2 mm so it is no longer under the periosteum. After careful aspiration, 1.5 ml of solution may be deposited. As the needle is being removed, when it is approximately halfway out, the lingual nerve is injected with the remaining solution, unless a buccal nerve block will be performed too. In that case, a few drops of local anesthetic should be reserved. Frequently, even without this last step, the lingual nerve will be anaesthetised.
Inferior Alveolar Nerve Block has the highest frequency of clinical failures of all intraoral injections. Thus, this block technique is not ideal to physically challenged or children. Moreover, Bilateral IA Nerve Block is rarely used other than for bilateral mandibular surgeries because anaesthetised soft tissue is often injured which results for the patient to have difficulty in swallowing and occurrence of trismus.
In case there’s a need to block multiple mandibular anterior teeth, use the IA Nerve Block on the side of most affected tooth and administer an incisive block on the other side.
The Inferior Alveolar Nerve Block injection anaesthetises the following areas:
- Mandibular Teeth from the Third Molar to the Midline
- Buccal Soft Tissue from the Premolars Anteriorly
- Body of the mandible
- Periosteum
- PDL
- Skin and Subcutaneous Tissues of the Chin and Lower Lip
- All on the Ipsilateral Side
LINGUAL NERVE BLOCK
The lingual nerve block is a supplemental block from Mandibular Nerve Block. This is done with a point of insertion of needle distally at 6-8 mm inferior to the lingual gingival margin of the second lower molar. The barrel of the syringe is place dover the contralateral incisor/canine region that’s angulated toward the second molar. The target area is the lingula nerve in the third molar region with the depth of penetration of the needle at 5-8 mm. The volume of anaesthetic solution injected is around 0.5 cc.
The Lingual Nerve Block injection anaesthetises the following areas:
- Lingual Gingiva
- Mucosa of the Anterior 2/3 of the Tongue
- Floor of Mouth
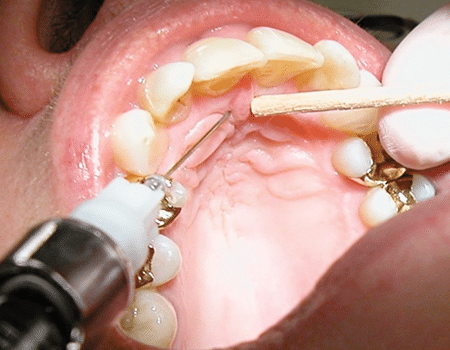
LONG BUCCAL NERVE BLOCK
Also known as simply the Buccal Nerve Block. The needle is inserted into the tissue at the distobuccal vestibule opposite to the second or third mandibular molar just medial to the coronoid notch until bone is contacted at approximately 1 to 3 mm, and a 0.25 ml of anesthetic solution is deposited.
The Buccal Nerve Block (Long Buccal Nerve Block) injection anaesthetises the following areas:
- Buccal Soft Tissue Lateral to the Mandibular Molars
GOW-GATES NERVE BLOCK
This technique was first published in 1973. Significantly the Gow-Gates technique offers better success over the IA nerve block. Its lower incidence of positive aspiration, and the absence of problems with accessory sensory innervation to the mandibular teeth.
The block is performed by having the patient open the mouth as widely as possible to rotate and translate the condyle forward. The condyle is palpated with the fingers of the non-dominant hand while the cheek is retracted with the thumb. Beginning from the contralateral canine, the needle is positioned so that a puncture point is made approximately at the location of the distobuccal cusp of the maxillary second molar. A 25-gauge long needle is inserted slowly to a depth of 25 to 30 mm; the endpoint is inferior and lateral to the condylar head. The injection must not be performed unless bone is contacted to ensure proper needle placement. After the needle is withdrawn 1–2 mm, the clinician aspirates and slowly injects the contents of the cartridge. This technique is unique among intraoral injections because the operator does not attempt to get as close as possible to the nerve to be anaesthetised. In fact, the needle tip should be approximately 1.0 cm directly superior to the nerve, in the superior aspect of the pterygomandibular space.
The Gow-Gates Nerve Block injection anaesthetises the following areas:
- Inferior Alveolar Nerves
- Lingual Nerves
- Auriculotemporal
- Buccal Nerves
- Mylohyoid Nerves
- Mandibular Teeth to the Midline
- Buccal Mucoperiosteum and Mucous Membranes on the Side of Block
- Anterior 2/3 of the Tongue
- Floor of the Oral Cavity
- Lingual Soft Tissues
- Periosteum
- Body of the Mandible
- Inferior Portion of the Ramus
- Skin over the Zygoma
- Posterior Portion of the Cheek
- Temporal Regions
The injection blocks the nerves at a point that is proximal to their division into inferior alveolar, buccal, and lingual nerves. The needle endpoint is the lateral aspect of the anterior portion of the condyle, just inferior to the insertion of the lateral pterygoid muscle. Using the intertragic notch as an extraoral landmark to help reach the neck of the mandibular condyle.
VAZIRANI-AKINOSI NERVE BLOCK
This another version of IA nerve block, also known as the Closed-Mouth Mandibular Block or Tuberosity Technique. This type of block is effective for patients with trismus or difficulty in opening the mouth.
Using a 25-gauge long needle, it is inserted parallel to the maxillary occlusal plane at the height of the maxillary buccal vestibule. The bevel should be oriented away from the bone of the mandibular ramus so that deflection occurs toward the ramus. The depth of penetration is approximately half the mesiodistal length of the ramus, which is about 25 mm in adults (measured from the maxillary tuberosity). The depth of insertion will vary with the anteroposterior size of the patient's ramus.
It is important to take note that this technique is quite challenging because of absence of bony endpoint. However, in adult patients, the rule of thumb is that the hub of the needle should be opposite to the mesial aspect of the maxillary second molar. After aspiration, the contents of the cartridge can be deposited slowly.
The Vazirani-Akinosi Nerve Block injection anaesthetises the following areas:
- Inferior Alveolar Nerves
- Incisive Nerves
- Lingual Nerves
- Buccal Nerves
- Mylohyoid Nerves
- Mandibular Teeth to the Midline
- Body of the Mandible
- Inferior Portion of the Ramus
- Buccal Mucoperiosteum
- Mucous Membrane Anterior to the Mental Foramen
- Anterior 2/3 of the Tongue
- Floor of the Oral Cavity
- Lingual Soft Tissues
- Periosteum
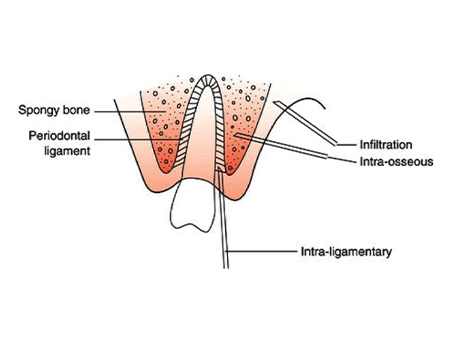
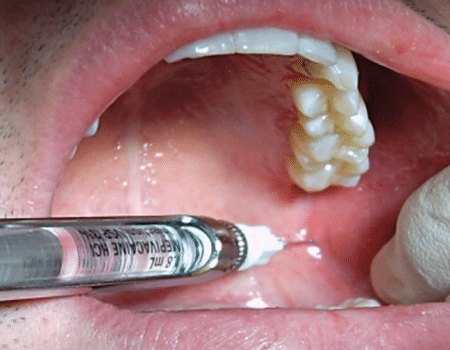
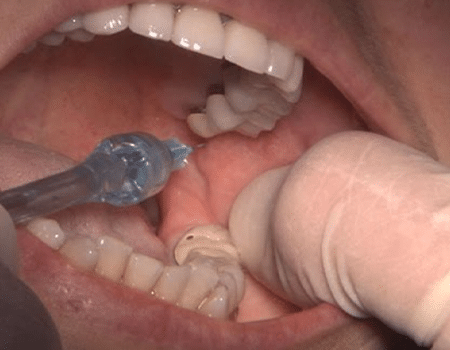
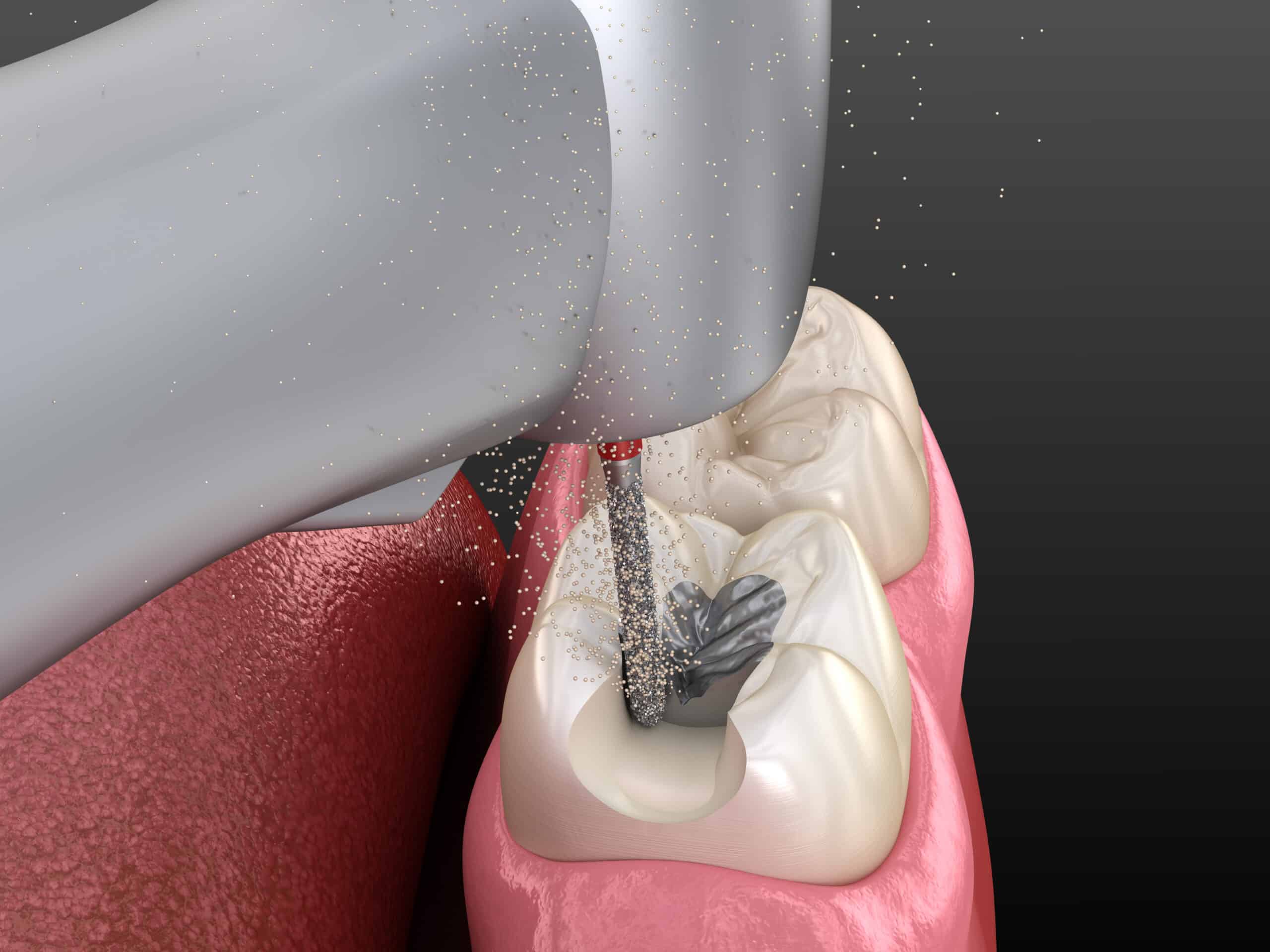
INTRAOSSEOUS NERVE BLOCK
This is used when a conventional block and infiltration injections are ineffective.
Intraosseous anesthesia requires the use of a round bur to provide a small dimple into interseptal bone. Once the hole had been made, a needle will be inserted into this hole and local anesthetic is deposited. Then, a handpiece-driven perforator and a solid 27-gauge wire with a beveled end that is activated and drills a small hole through the cortical plate. The anesthetic solution is delivered to cancellous bone through the 27-gauge ultrashort injector needle placed into the hole made by the perforator
The site for this technique is 2 mm apical to the intersection of lines drawn horizontally along the gingival margins of the teeth and a vertical line through the interdental papilla. The site should be distal to the tooth to be treated, and care should be taken to avoid the area of the mental foramen. The amount of anesthetic injected ranges from one third to three quarters or 0.6 to 1.2 ml of the cartridge. The onset of anesthesia is immediate, and pulpal anesthesia will last for 15–45 minutes.
The Intraosseous Anaesthesia injection anaesthetises the following areas:
- Single Tooth or Multiple Teeth in One Quadrant
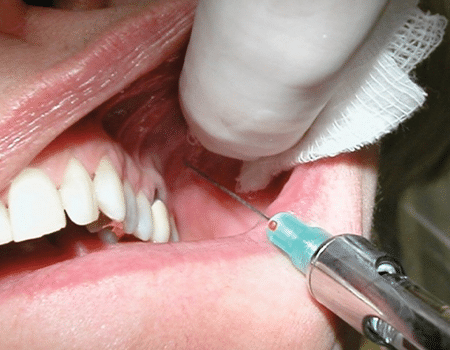
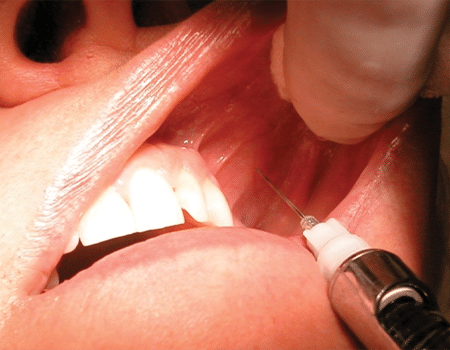
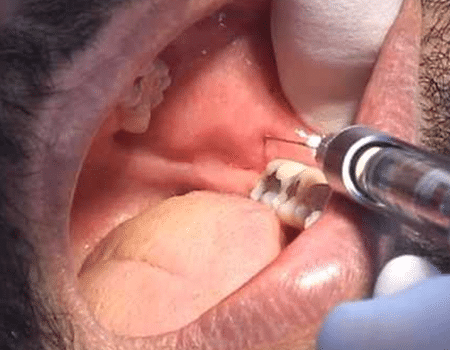
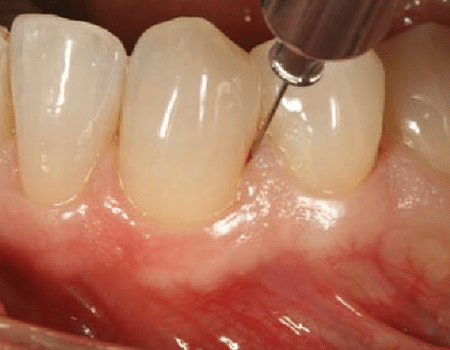
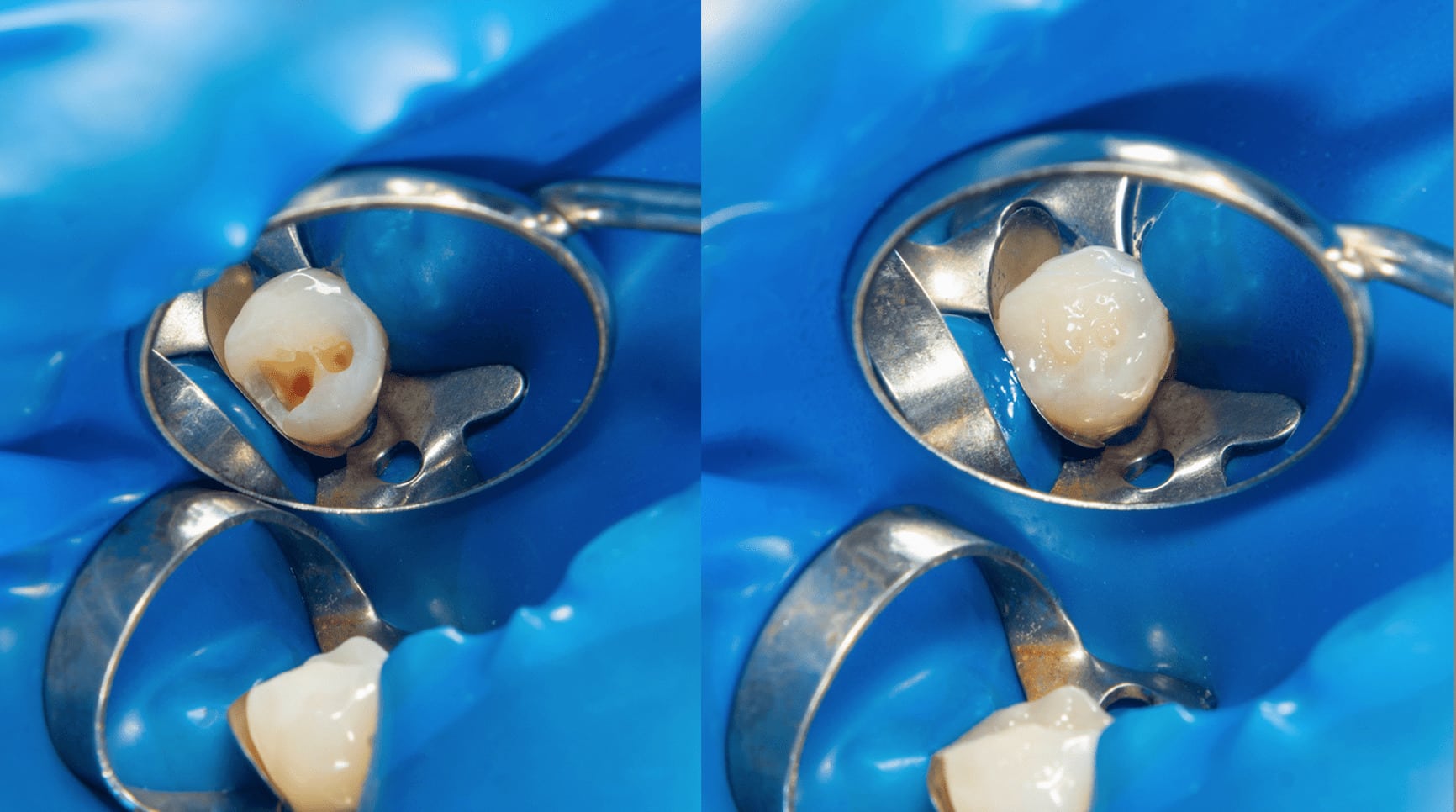
PERIODONTAL LIGAMENT BLOCK
The PDL Block method of anaesthetising an individual tooth is utilized to avoid the undesirable consequences of regional block anesthesia.
A 27-gauge short needle with the bevel toward the tooth is inserted through the gingival sulcus on the mesial of the tooth to be anaesthetised and inserted as far apically as possible. Approximately 0.2 ml of anesthetic solution is deposited over a minimum of 20 seconds. Then, the same technique is performed on the distal of the tooth. This technique may be uncomfortable if the rate of injection is too rapid or the tissues are inflamed. The duration of pulpal anesthesia is extremely variable, so repeated PDL block may be necessary to complete a procedure.
INTRAPULPAL ANESTHESIA
Anaesthesia during an Endodontic procedure may not be easily obtained. Once the pulp has been exposed, anaesthetic may be placed directly into the pulp.
A 27-gauge short needle is inserted into the pulp chamber and wedged firmly into the root canal. A small volume of 0.2 to 0.3 ml of local anaesthetic is injected. While this technique may prove uncomfortable for the patient, it invariably works to provide effective pain control. In most cases, the duration is adequate to permit extirpation of the pulpal tissues.
CONCLUSION
We know that administration of local anaesthesia is something we regularly do. In fact, it becomes second nature to us, but, we are still human and can commit mistakes. It helps that we refresh ourselves with what’s basic and may even learn something new from this post. We must be humble enough to constantly educate ourselves to render our dental treatments at its utmost safety to our patients.
CONTRIBUTORS:
Dr. Bryan Anduiza – Writer
Dr. Jean Galindez – Editor | Writer
REFERENCES:
1. Kenneth L. Reed, DMD,* Stanley F. Malamed, DDS,† and Andrea M. Fonner, DDS: Local Anaesthesia Part 2: Technical Considerations
2. Gow-Gates GAE: Mandibular conduction anaesthesia: a new technique using extraoral landmarks. Oral Surg 1973;36:321–328
3. Akinosi JO: A new approach to the mandibular nerve block. Br J Oral Maxillofacial Surg 1977;15:83–87
4. Snell RS: Clinical Anatomy for Medical Students, 5th ed. New York: Little, Brown, 1995
5. McDaniel WM: Variations in nerve distributions of the maxillary teeth. J Dent Res 1956;35:916–921
6. Heasman PA: Clinical anatomy of the superior alveolar nerves. Br J Oral Maxillofacial Surg 1884;22:439–447
7. Loetscher CA, Walton RE: Patterns of innervation of the maxillary first molar: a dissection study. Oral Surg Oral Med Oral Pathol 1988; 65:86–90
8. Malamed SF, Trieger N: Intraoral maxillary nerve block: an anatomical and clinical study. Anaesthesia Program 1983;30:44–48
9. Poore TE, Carney F: Maxillary nerve block: a useful technique. J Oral Surg 1973;31:749–755
10. Malamed SF: Handbook of Local Anesthesia, 4th ed. Maryland Heights, MI: Mosby, 1997
11. Case of the week: Kathy Bassett Demonstrates the Gow- Gates Injection https://www.youtube.com/watch?v=SBbRQODpsJg
12. Lehtinen R. Penetration of 27- and 30-gauge needles. Int J Oral Surg. 1983;12:444–445
13. Browbill JW, Walker PO, Bourcy BD, et al. Comparison of inferior dental nerve block injections in child patients using 30-gauge and 25-gauge short needles. Anesth Prog. 1987;34:215–219. 8
14. Lipp MD. Local Anesthesia in Dentistry. Vol. 106 Chicago: Quintessence Publishing; 1993. [Google Scholar]
15. Phillips WH. Anatomic considerations in local anesthesia. J Oral Surg. 1943;1:112–121
16. Malamed SF. Handbook of Local Anesthesia. 5th ed. St Louis: The CV Mosby Co; 2004
17. Jastak JT, Yagiela JA. Regional Anesthesia of the Oral Cavity. St Louis: The CV Mosby Co; 1981
18. Malamed SF: Handbook of Local Anesthesia, 4th ed. Maryland Heights, MI: Mosby, 1997
19. Evers H, Haegerstam G. Introduction to Dental Local Anesthesia. 2nd ed. St Louis: The CV Mosby Co; 1990
20. Watson JE. Appendix: some anatomic aspects of the Gow-Gates technique for mandibular anesthesia. Oral Surg Oral Med Oral Pathol. 1973;36:328–330
21. Reed KL. Advanced techniques of local anesthetic injection. Gen Dent. 1994;42:248–251
23. Haas DA. Alternative mandibular nerve block techniques: a review of the Gow-Gates and Akinosi-Vazirani closed-mouth mandibular nerve block techniques. J Am Dent Assoc. 2011;142:8S–12S
24. Moore PA, Cuddy MA, Cooke MR, Sokolowski CJ. Periodontal ligament and intraosseous anesthetic injection techniques: alternatives to mandibular nerve blocks. J Am Dent Assoc. 2011;142:13S–18S
25. Meechan JG, Ledvinka JI. Pulpal anesthesia for mandibular central incisor teeth: a comparison of infiltration and intraligamentary injections. Int Endod J. 2002;35:629–634